Author: Fraence Hardtstock MSc * 1, Zaza Katsarava MD, PhD, Prof 2-5, Thomas Wilke PhD, Prof 6, Zeki Kocaata PhD 1, Tim Kirchmann Diploma 7, Ulf Maywald PharmD, MPH 8, Alice Eberhardt PhD 7
Author Affiliation:
1 Ingress-Health HWM GmbH, Alter Holzhafen, Germany
2 Dept. of Neurology, Evangelical Hospital Unna, Germany
3 Dept. of Neurology, University of Duisburg-Essen, Germany
4 EVEX Medical Corporation, Tbilisi, Republic of Georgia
5 IM Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russian Federation
6 IPAM e.V., affiliated institute of the University of Wismar, Germany
7 AbbVie GmbH, Wiesbaden, Germany
8 AOK PLUS, Dresden, Germany
Competing Interests: The author/s declare no competing interests.
Issue: 04.04
DOI: 10.30756/ahmj.2020.04.04
Received: Nov 26, 2020
Revised: Jan 25, 2021
Accepted: Jan 26, 2021
Published: Feb 4, 2021
Recommended Citation: Hardtstock F, Katsarava Z, Wilke T, et al. Real-world treatment and associated healthcare resource use among migraine patients in Germany. Ann Head Med. 2020;04:04. DOI: 10.30756/ahmj.2020.04.04
Background: In order to evaluate unmet therapeutic need, this study sought to describe treatment patterns, as well as associated healthcare resource use (HCRU) and costs incurred by migraine patients in Germany.
Methods: We conducted a retrospective analysis of a German claims dataset from 2013-2017, including over three million publicly-insured patients. Adult patients were included if they received at least one inpatient and/or two confirmed outpatient claims for headache/migraine from 2013-2016. Using prescription data from 2017, patients were separated into four main cohorts: those receiving prescriptions for (1) acute agents only, (2) prophylactic agents only, (3) both acute and prophylactic agents, and (4) neither acute nor prophylactic agents. Baseline characteristics were observed from 2013-2016; treatment and HCRU/cost outcomes were assessed in 2017.
Results: In total, 199,283 patients were included in this analysis (mean age, 49.49 years; 73.04%, female) and 9,005 prophylactic therapy starters were identified. Overall, 43.47% of migraine patients did not receive acute or prophylactic medication in 2017, while 33.81% received only acute treatment, 9.45% received only prophylactic medication and 13.28% received both. Only 28.90% of patients initiating a prophylactic treatment were persistent after two years. HCRU was elevated for all groups, while direct costs ranged from €2,288-7,246 per year, and indirect costs ranged from €868-1,859.
Conclusions: Despite high levels of HCRU, few migraine patients were treated with prophylactic agents, and those who did were at an elevated risk of early discontinuation. Ultimately, these findings indicate a resounding need for safe, timely, and efficacious use of prophylaxis among migraine patients.
Background
Migraine is one of the most frequently disabling neurological diseases and is the leading cause of disability in adults under the age of 50 1. In 2016, migraine was found to be the leading driver of years lived with disability (YLD) worldwide in the age group of 15 to 49 years 2. Since migraine primarily affects people in their productive years (from a labor market perspective), it leads to substantial productivity losses, and therefore constitutes a serious public-health concern 3, 4, 5.
Pharmacological treatment of migraine often includes use of acute therapies, which aim to relieve symptoms during attacks, as well as preventive or prophylactic therapies in order to decrease the severity and frequency of attacks 6, 7. In addition, several non-pharmacological approaches such as acupuncture and psychotherapy may be considered as treatment options 4, 8. Migraine is recognized as an area of significant unmet therapeutic need, as it relates to the underdiagnosis and widespread undertreatment of patients 9, 10. There are a number of reasons for the undertreatment of patients with prophylactic therapies, including the misdiagnosis of many migraine patients with general headache [9]. Ultimately, correct diagnosis and assessment of disease type, as well as the intensity and frequency of attacks, is essential to facilitate appropriate management of migraine 7, 11.
Ultimately, there is very limited evidence on the treatment of migraine patients and associated healthcare resource utilization (HCRU) and costs in Germany. Nevertheless, these data are urgently needed to understand potential avenues for improving the real-world treatment of patients. This retrospective claims data analysis aimed to identify patients with headache and migraine in Germany, and to describe their acute and prophylactic drug treatment as well as HCRU, direct and indirect costs.
Methods
Study design and data source
This was a retrospective, non-interventional comparative cohort analysis of patients with migraine or headache, utilizing an anonymized routine dataset provided by AOK PLUS, a German public sickness fund insuring about 3.2 million persons in Germany. Complete statutory insurance data on all documented diagnoses (inpatient and outpatient), treatments and procedures, as well as pharmaceutical and non-pharmaceutical prescriptions for the period 2013-2017 were available. Furthermore, the dataset included information on the cost of prescriptions, hospitalizations, and rehabilitations, as well as outpatient physician visits. As the dataset was anonymized, no ethical approval was required. Approval from the data owner was provided prior to the start of the analysis, based on the submission of a study protocol. The study was led by a Scientific Steering Board, consisting of the authors of this publication.
Patient Eligibility Criteria
In order to describe treatment patterns and HCRU in 2017, patients were included if they received at least one inpatient and/or two confirmed outpatient diagnoses of headache (ICD-10 R51 and G44) or migraine (ICD-10 G43) from 2013-2016, and if they were at least 18 years of age and alive on 01/01/2017. Furthermore, patients must have been continuously insured from 2013-2017. Baseline characteristics such as sociodemographic profile, comorbidities, and type of diagnosing physicians (i.e., general practitioners, specialists) were observed from 2013-2016 in four main patient cohorts.
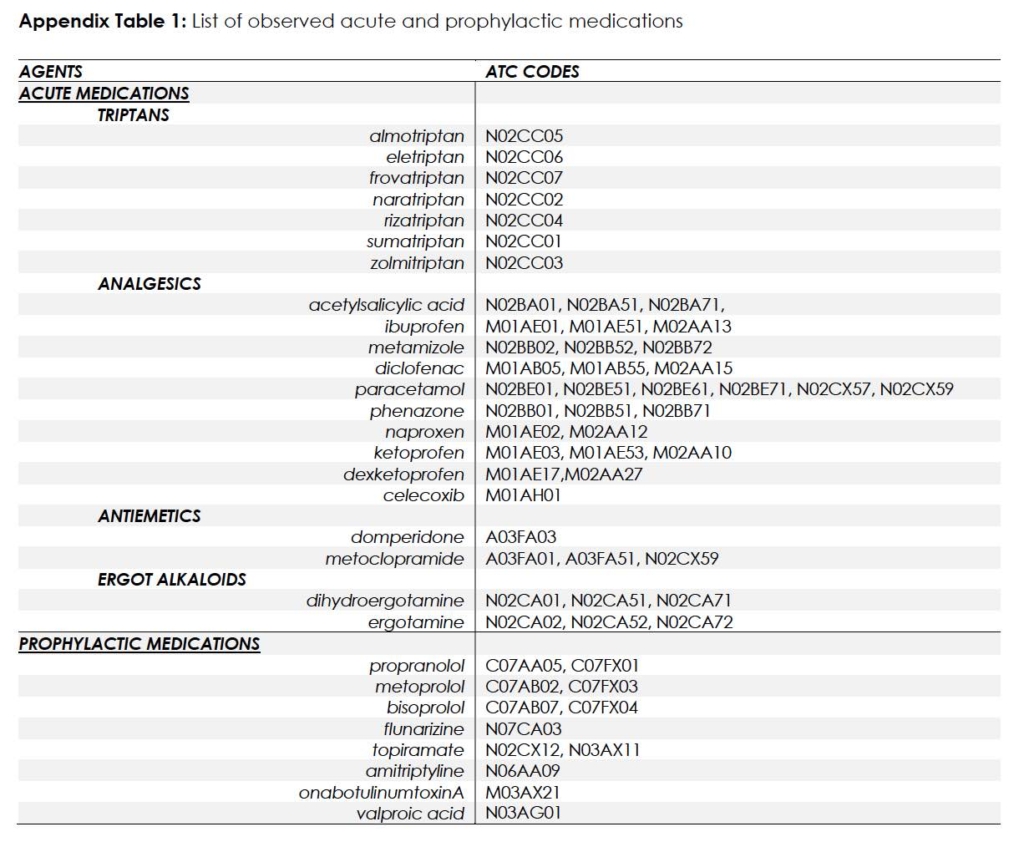
Analysis of Treatment Patterns
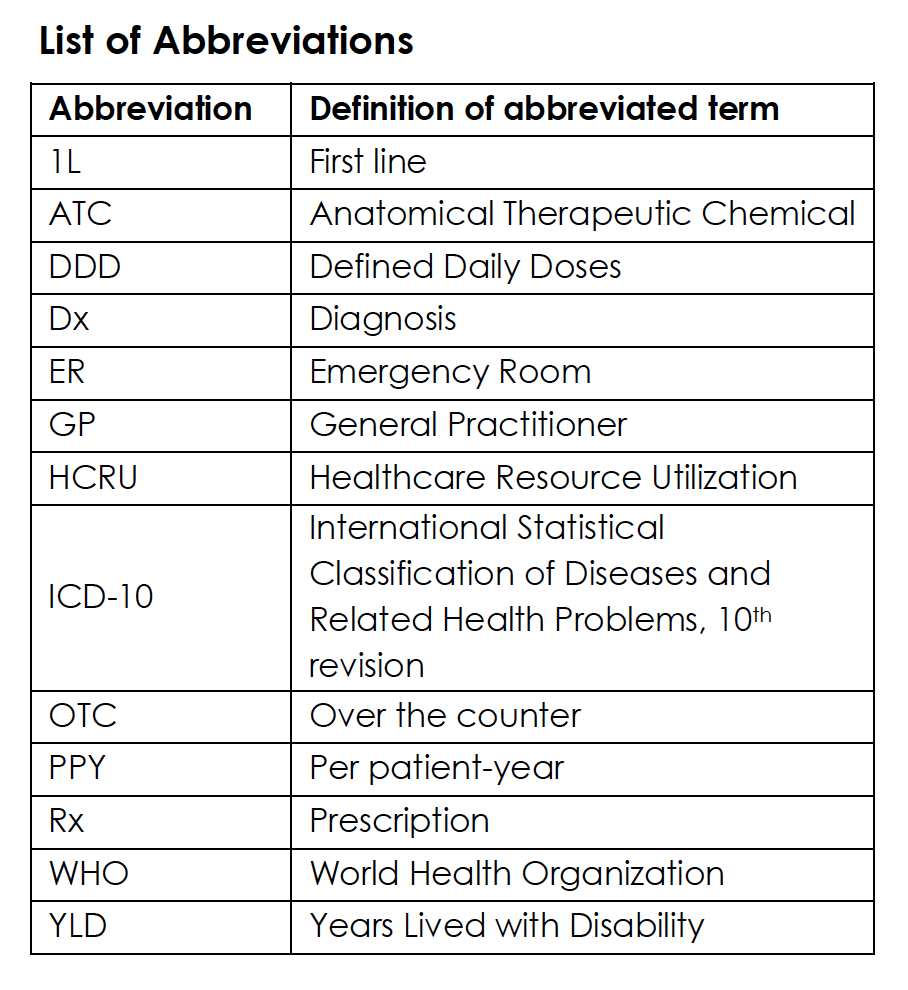
The number of prescriptions and average dosage received was calculated per agent as well as per drug class and reported for the four treatment cohorts. Each patient’s total prescription supply (measured in daily doses) was estimated based on the number of packages received by patients, each package’s size (e.g. number of tablets), the concentration of the active substance in each package, and the defined daily doses (DDD) for medications, according to the World Health Organization (WHO) 12.Both acute and prophylactic prescriptions (Rx) were analyzed in the observational year 2017 to group patients based on their medication therapy. Data on over the counter (OTC) drugs were not available. The study considered a range of acute medications including triptans, analgesics, antiemetics and ergot alkaloids, as well as prophylactic agents which included propranolol, metoprolol, bisoprolol, flunarizine, topiramate, amitriptyline, onabotulinumtoxinA, and valproic acid. A list of all observed acute and prophylactic agents and their respective anatomical therapeutic chemical (ATC) codes is presented in Appendix Table 1. Patients were assigned to one of four main cohorts, based on the type of Rx treatment they received in 2017, including: neither acute nor prophylactic medication (cohort N), only acute medication (cohort A), only prophylactic medication (cohort P), or both acute and prophylactic medication (cohort AP) (Figure 1).
Figure 1: Study design scheme of HCRU/cost analysis in 2017
In a separate analysis, migraine/headache patients who began receiving prophylactic treatment in 2014-2015 were observed in order to identify treatment lines, switches, and treatment discontinuation in the period following initiation of treatment. Patients who began receiving prophylactic treatment (including at least one of the above prophylactic agents) between 01/01/2014-31/12/2015 and had no prophylactic treatment history in 2013 were included in the analysis. The first prescription for prophylactic treatment was considered as the index date and all patients were observed for 24 months after initiation of therapy. Discontinuation of therapy was considered, when a patient did not refill a prescription for his/her prophylactic medication within 180 days of the last expected drug coverage date of the last observed prescription.
In addition, an exploratory analysis was performed to estimate the number of patients with migraine/headache who did not receive prophylactic medication in 2016 but may have benefited from such a therapy. A potential need for a prophylactic medication was defined as having received triptans in the amount of >8 daily dosages per month in 2016, or alternatively >5 daily dosages per month in combination with either (i) an emergency room (ER) visit with a diagnosis of headache/migraine, (ii) at least one migraine/headache-associated hospitalization, or (iii) an inpatient rehabilitation stay associated with headache/migraine in 2016. For all patients with an identified need for prophylactic therapy in 2016, prescriptions of prophylactic medications were observed in 2017.
Analysis of HCRU And Cost
The following HCRU variables were observed and reported per patient-year (ppy): inpatient hospitalizations, outpatient physician visits, inpatient rehabilitation stays, physiotherapy prescriptions, prescribed aids and remedies, acupuncture prescriptions, and days absent from work. Overall costs (€) were reported ppy for the following categories: (i) outpatient visits [based on documented ‘treatment points’ for outpatient physician visits], (ii) outpatient prescriptions [based on official retail list prices for outpatient medication prescriptions], (iii) hospitalizations, including procedures and medications [based on diagnosis-related group reimbursements for inpatient hospitalizations], (iv) inpatient rehabilitations [directly covered in the database], and (v) prescriptions of aids and remedies [based on prices, which are directly covered in the database]. Since patient-specific salaries were not available in the database, indirect costs related to loss of productivity were approximated based on the number of days absent from work, multiplied by age- and gender-specific average gross salaries in Germany 13. HCRU and cost analyses were repeated for the exploratory cohort of patients who did not receive prophylactic treatment in 2016, but may have benefited from it (i.e. those receiving >8 daily dosages of triptans per month or >5 daily dosages in combination with further criteria as previously described).
Results
Patient characteristics
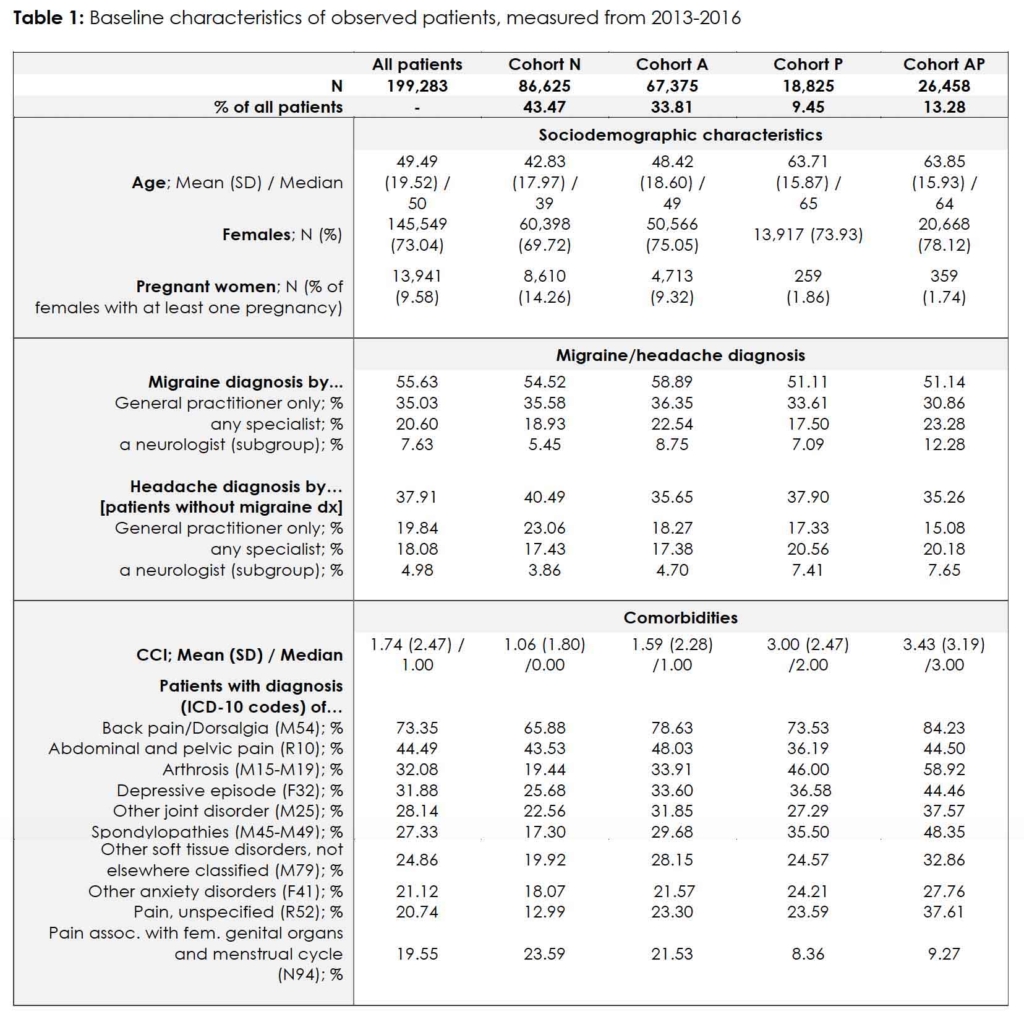
We identified 199,283 patients with headache and/or migraine in our database (mean age 49.49 years; 73.04% women; Table 1). Among patients included in the study, 6.46% did not receive an outpatient diagnosis of migraine or headache but were diagnosed with headache/migraine at least once during an inpatient stay, while 93.54% of the patients were diagnosed in an outpatient setting (55.63% with migraine diagnoses and 37.91% with headaches but not migraine).
Most observed comorbidities in the identified headache/migraine patients included back pain (73.35%), abdominal and pelvic pain (44.49%), arthrosis (32.08%) and depression (31.88%). Patients without any prescription of acute or prophylactic medication (cohort N) were younger (mean age 42.83 vs. 48.42-63.85), less often female (69.72% vs. 73.93%-78.12%), and with less severe comorbidities (mean CCI 1.06 vs. 1.59-3.43) than patients receiving acute medication (cohort A), prophylactic medication (cohort P) and/or acute and prophylactic medication (cohort AP).
Treatment Patterns
Cross-sectional analysis 2017
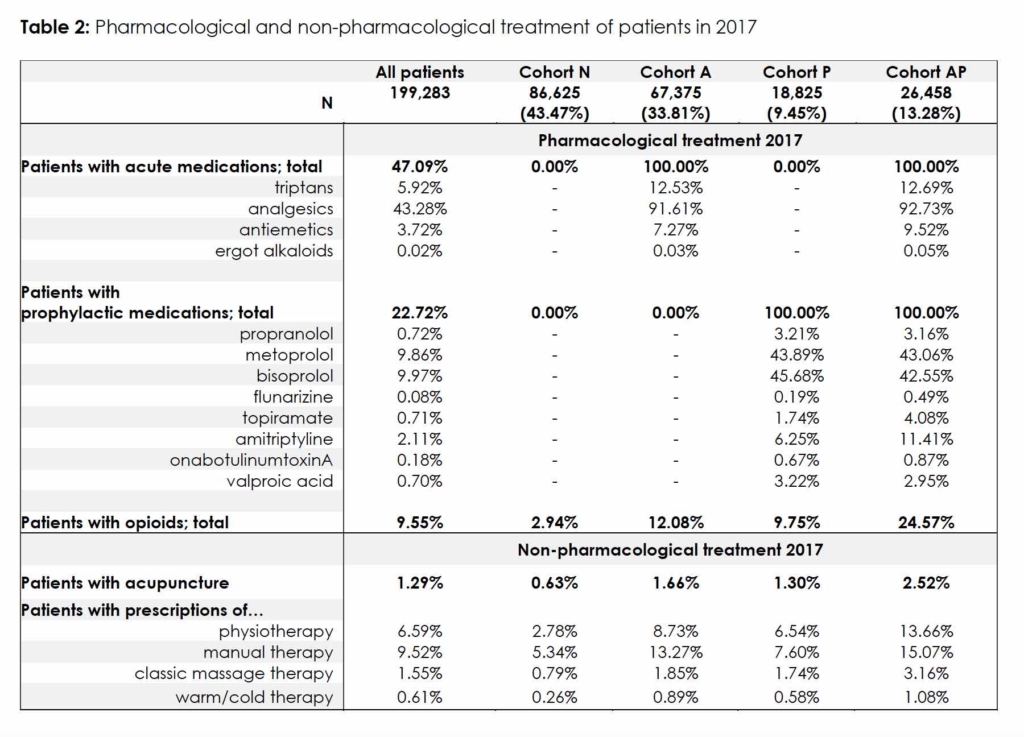
Overall, 43.47% of all observed patients (86,625/199,283) did not receive prescriptions for acute or prophylactic medication in 2017 (cohort N). In 67,375 (33.81%) of all observed patients, only prescription of acute medications was observed (cohort A), with 12.53% receiving triptans. Patients who only received prophylactic medication and no acute medication accounted for 9.45% of the observed cohort (18,825/199,283; cohort P), among which most received either metoprolol (43.89%) or bisoprolol (45.68%). All remaining patients (13.28%; 26,458/199,283) received both acute and prophylactic therapy (cohort AP), among which 12.69% received triptans. The number of patients receiving opioids varied among each group, ranging from 2.94% in cohort N to 24.57% in cohort AP.
In addition to pharmacological treatment of migraine, other forms of non-pharmacological treatment were also analyzed. Only a small proportion of patients in the study received a prescription for acupuncture (1.29%) or for physiotherapy (6.59%). In cohorts receiving acute treatment for migraine (cohorts A and AP), a higher percentage of patients was found to receive non-pharmacological therapies (as compared to patients in cohorts N and P) (Table 2).
Longitudinal Analysis of Prophylactic Therapy Starters
For the longitudinal analysis, 9,005 patients who began receiving prophylactic treatment in 2014-2015, were identified in the database. Their mean age at initiation of therapy was 52.19 years, and 78.48% of observed patients were women. Most of these patients started therapy with bisoprolol (33.97%), followed by metoprolol (31.17%) and amitriptyline (21.11%). Other prophylactic agents used in treatment included topiramate (5.97%), propranolol (3.75%), valproic acid (1.19%), flunarizine (0.73%), onabotulinumtoxinA (0.48%) or any combination of the agents mentioned above (1.62%).
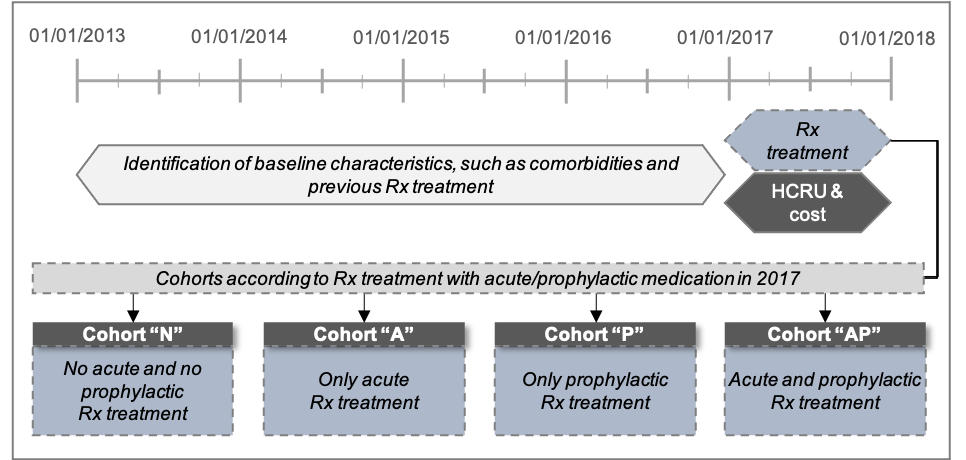
Among this group, 5,726 patients (63.59%) received at least one prescription for acute medication in the 12 months prior to initiation of prophylactic therapy. Of those, 1,399 patients received triptans. For the latter, on average, triptans were available for 4.71 days per month. In contrast, during the first 12 months after initiation of prophylactic therapy, 5,698 patients (63.28%) received acute medications. Here, 1,432 patients received at least one prescription of triptans, with 4.85 days per month of available triptans (Figure 2).
Figure 2: Acute medications before and after start of prophylactic 1L treatment
Overall, 2,602 patients (28.89%) continued their first-line prophylactic therapy for at least two years following initiation, while 930 patients (10.33%) switched to another second-line prophylactic therapy, and 5,473 patients (60.78%) discontinued their first-line therapy without starting a new prophylactic therapy. Time until discontinuation for the last group of patients was on average 112 days.
Exploratory Analysis of Patient’s Needs for Prophylactic Medication
Among all 199,283 observed patients, 154,131 (77.34%) did not receive a prescription for prophylactic medication in 2016. In the same year, 948 of those patients received >8 daily dosages of triptans per month, while an additional 32 patients received >5 daily dosages of triptans and experienced at least one migraine/headache-associated ER visit, hospitalization or inpatient rehabilitation stay. Among these 980 patients, a minority of 115 patients (11.7%) received a prophylactic medication in 2017.
HCRU And Costs in 2017
HCRU
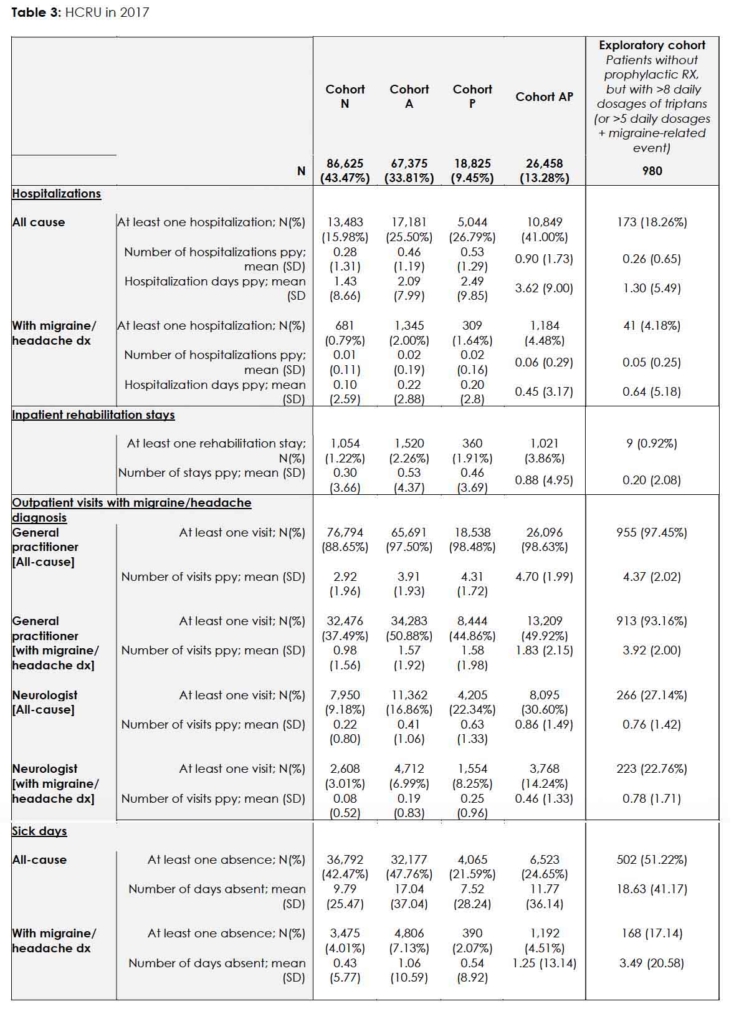
For nearly all observed HCRU/cost variables, a higher utilization was found in patients receiving prophylactic treatment (cohorts AP and P), compared to patients without medication (cohort N) or with only acute Rx (cohort A). HCRU and cost were also reported for the exploratory cohort of 980 patients expected to benefit from prophylactic treatment (those who received substantial monthly doses of triptans, but no prophylactic Rx). In these patients, migraine/headache related HCRU was comparatively high (Table 3).
On average patients in cohort AP were hospitalized (for any cause) around 0.90 times per year, a rate which is over three-fold higher than that which was observed in patients from cohort N who received no treatment (0.28 ppy). Furthermore, migraine/headache-related hospitalizations were 0.06 ppy in cohort AP as compared to 0.01 ppy in cohort N. In the cohort of 980 patients with no prophylactic treatment but high triptan use, the rate of migraine/headache-related hospitalizations was 0.05 ppy.
The number of patients with sick leave and the number of days of sick leave were both higher in patients from cohort A, in comparison to patients who received a prophylactic medication (cohorts AP and P). Patients in cohort A took on average 17.04 days of sick leave (1.06 days related to migraine and/or headache), compared to an average of 7.52 days (0.54 days) in patients from cohort P, and 11.77 days (1.25 days) in patients from cohort AP. For the exploratory cohort of 980 patients, the number of patients who had at least one absence (51.22%) was higher than in all other cohorts (21.59%-47.76%). Furthermore, for this cohort, the number of days of missed work due to migraine/headache was 3.94 days ppy, and therefore significantly higher than in all other cohorts (0.43-0.54 days ppy).
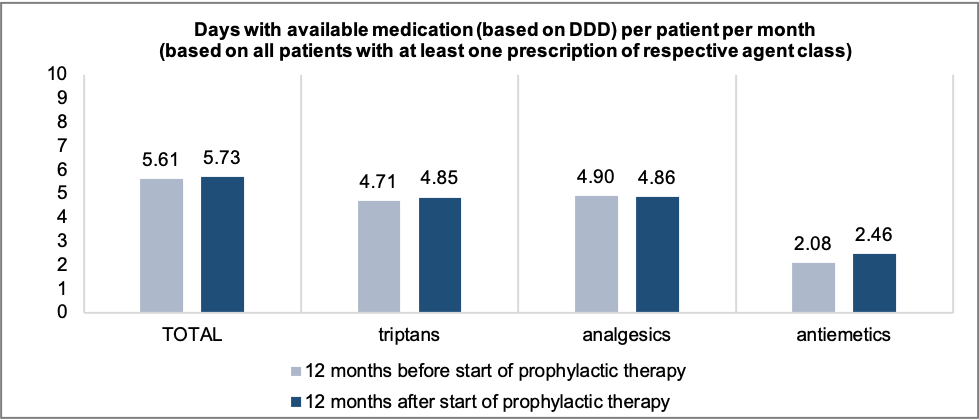
Cost
Total (all cause) direct costs ppy ranged from €2,288.14 in cohort N to €7,246.18 in cohort AP, as indicated in Figure 3. Hospitalizations accounted the largest share of costs in all cohorts (38.81%-46.24% of total direct costs), except for in the explanatory cohort (22.69%), where outpatient visits and prescriptions accounted for a higher proportion of total direct costs. Rehabilitation stays had the lowest impact on overall direct costs comprising only 0.86%-2.22%. On average, patients in Cohort AP incurred the highest direct costs across all categories, while patients in cohort N incurred the lowest. Indirect costs associated with loss of productivity due to days absent from work were lowest in cohort P (€868.19 ppy) and highest in cohort A (€1,861.24 ppy); patients in the exploratory cohort incurred an indirect cost of €2,031.73 ppy.
Figure 3: Costs in 2017 per patient-year in €
Discussion
Summary and Comparison of Findings With Existing Literature
In this study, we analyzed patients with headache/migraine in a real-world setting in order to increase knowledge related to current treatment patterns of these patients in Germany. The goal of this research is to outline ongoing challenges related to the diagnosis and treatment of migraine patients in order to pave the way for improvements in medical care for patients with migraine.
Management of migraine and headache is multidimensional. Emphasis should be placed upon educating patients about appropriate use of OTC medication, improving the quality of advice provided to patients by pharmacists, as well as integrating, coordinating and synchronizing services offered by primary healthcare providers as well as specialists. Around 50% of migraine patients with relatively mild and infrequent attacks attempt to independently manage their disease through use of OTC remedies, and thus may not consult a physician. Nevertheless, at least 50% of patients require some degree of medical follow-up or consultation 14. To a large extent, demand for clinical consultations among migraine patients is driven by the inefficacy of OTC drugs and the resulting need for prescription treatment. It has been previously reported that up to one-third of all migraine patients who suffer from frequent migraine attacks, are probably in need of prophylactic medication 7. It is particularly important for these patients to receive adequate treatment to improve clinical outcomes, well-being, and productivity in the workplace 15, 16. Our findings indicate that, even in a relatively well-resourced country like Germany, only a small portion of patients expected to benefit from migraine medication actually receive treatment.
Our study reveals that nearly half of all patients with migraine/headache diagnoses did not receive any prescription of acute or prophylactic medication in 2017 (43.47%). Approximately one-third of the patients received only acute medications (33.81%) and just one fifth (22.72%) were prescribed prophylactic agents. Our exploratory analysis of patients who heavily depend on prescribed triptans (>8 daily dosages per month or >5 daily dosages per month with additional indicators of high disease severity) revealed a stark unmet need for prophylactic agents, since less than 10% of these patients received subsequent prescriptions for prophylactic medication. These findings align with those of previous studies which have demonstrated generally poor treatment patterns and disease performance in headache/migraine patients throughout Germany and elsewhere in Europe. A recent medical chart review reported that 27.5%-58.4% of migraine patients do not receive any therapy 17, while a study of 8,000 migraine patients from 10 EU countries confirmed that very few patients received adequate migraine-specific treatment including both, acute and prophylactic medications [3]. Further to these findings, one study in Germany demonstrated an overall low frequency of migraine-specific prescriptions, especially among general practitioners (GPs) 17.
However, reasons for the low quality of care afforded to migraine and headache in patients throughout Germany and across the world are manifold. Despite the fact that migraine is highly prevalent and is associated with huge adverse consequences for affected people and the society, it is generally not considered a significant medical problem by patients, healthcare providers and health policymakers 18. Oftentimes people affected by migraine are not aware of their disease and thus, do not consult a doctor to receive a diagnosis or proper treatment for their symptoms. One study provided evidence that awareness of migraine was low among both affected patients and healthcare providers 19. These findings were corroborated by a study in France which indicated that 60% of 10,000 patients with migraine were unaware of their diagnosis 20. With this in mind, we acknowledge potential underestimation of unmet need in our patient population, since not all patients in need of therapy will have visited physicians during the study period and, therefore, were not included in this analysis. A previous study in Germany provided evidence that only 42% of patients with migraine consulted a physician, while a clear majority of patients relied exclusively on OTC medications, despite reporting symptoms 21. This presents a limitation of the present study, as data on OTC medication use for our patient population were not available in the dataset.
In addition to the potential lack of awareness regarding migraine diagnoses, some GPs and specialists may not perceive headaches to be medically important enough to spend time diagnosing/treating symptoms, providing patients with detailed advice, or following-up with regard to the presentation of new symptoms. A study conducted in 10 headache centers in Italy revealed that only 26.8% of patients with migraine had received a previous diagnosis that was correct 22. Another multinational study found that only 28 percent of migraine patients (who were subsequently referred to specialized headache centers) had been diagnosed with migraine by their treating GPs 23. Furthermore, as shown by a study conducted in the UK, some GPs do not follow established treatment guidelines when patients with headache symptoms attend their practice 24. As a consequence, patients receive either no treatment or improper treatment, as demonstrated in the Europe-wide EUROLIGHT study 3.
However, among patients who received a new prescription for prophylactic therapy in our study (N = 9,005), 60.78% discontinued prophylactic treatment within two years, without re-initiation. Ultimately, low medication compliance constitutes another key driver of poor medical care and high unmet need among patients. Poor adherence to prophylactic medication for migraine has been observed in previous research and was shown to result from insufficient effectiveness and/or treatment-related side effects 25, 26. One retrospective claims analysis in the US revealed that more than 80% of patients with chronic migraine discontinued treatment within twelve months 27, which is even higher compared to our findings. In contrast, the European-wide REPOSE study reported a lower persistence (22.7% discontinuation) for a cohort of patient with chronic migraine, who initiated a therapy with onabotulinumtoxinA 26. Although there may be differences in the level of adherence and persistence between different patient groups and therapeutic interventions, challenges related to treatment adherence and potential side effects signal an ongoing need for the improvement of migraine therapies, with regard to effectiveness and safety.
Our HCRU and cost analysis confirmed high levels of unmet need in a substantial proportion of observed patients, particularly in those who receive medications. According to our analysis, patients taking prophylactic medications were hospitalized more frequently and logged more sick days than patients who did not receive prophylactic treatment. Although this may be due in part to the likelihood of more severe cases among those who received prophylactic treatment, and these findings are likely biased by indication (i.e., higher proportion of migraine patients in this cohort), patients with prophylactic migraine medications had higher utilization of acute medications too, indicating a higher headache frequency. Unfortunately, no data on headache frequency among study participants was available in the database to confirm this. Generally, economic consequences of migraine, comprised of direct and indirect costs, are enormous.
Cost estimates are an important measure used to inform health policymaking via the estimation of expenses incurred by different healthcare services. In Europe, financial costs attributed to migraine are estimated to range between €50 and €111 billion, with direct and indirect costs accounting for 7% and 93% respectively 28. Direct costs incurred by healthcare services attributed to migraine, were found to be €1,222 per person 28. Another European study reported comparable average costs over three months, ranging from €373.8 in Germany to €929.6 in the UK 29. Indirect costs, as shown within these studies, constitute most of the economic burden, with productivity loss accounting for two-thirds of indirect costs 28. Our analysis confirmed that indirect costs (related to days absent from work) should not be neglected in analyses of migraine related HCRU and cost. On the contrary, it must be emphasized that average monthly costs associated with diminished productivity at work (presenteeism) are higher than those arising from sick leave (absenteeism) 30. However, an estimation of costs related to onsite productivity loss was not possible in this study and research in this area is generally limited.
Limitations
Strengths of this study include an absence of study site/patient selection bias, coverage of all inpatient and outpatient healthcare sectors, and utilization of a large cohort of 199,283 patients. Nevertheless, we acknowledge that some limitations may apply. First, generalizability of results could be affected by the fact that the health insurance fund which provided the data only covers patients in two regions of Germany (Saxony and Thuringia). However, since health reimbursement rules are identical across Germany, considerable differences in the management of migraine patients are not expected.
Second, information on the number of migraine attacks in the observed patient cohorts was not available. Since this information (as well as further clinical data) was missing, only ICD-10 codes could be used to identify the relevant patient population. However, the correct use of ICD-10 codes cannot be verified. Therefore, the patient population in this study includes those with a relatively wide range of headache disorders. Due to potential differences in the severity of patients’ conditions, not all patients may have been in need of prophylactic medication. To address this concern, an exploratory analysis was performed using a subgroup of patients who did not receive prophylactic medications but instead received a substantial amount of prescription triptans and/or experienced migraine-related events, indicating a demonstrated need for prophylactic medications.
Third, analysis of prophylactic treatment with monoclonal antibodies such as erenumab, galcanezumab and fremanezumab was not included as these medications were not available during the period of observation. Fourth, dosage as well as persistence analyses were conducted using data on filled prescriptions only. Information on unfilled prescriptions as well as OTC medications was not analyzed, as those data were not available in the relevant sickness fund dataset. Ultimately, the latter may have caused an underestimation of medication use in our patient population. Moreover, HCRU among headache/migraine patients may have been underestimated if alternate therapies not covered by the participating sickness fund were accessed by patients via alternate means (i.e., supplementary insurance, out-of-pocket payments, etc.). Fifth, this analysis was exclusively descriptive, and no adjusted analyses were performed. Finally, our HCRU and cost analysis was based on reimbursements only, which exclude patient co-payments. However, these costs are generally low in Germany.
Conclusions
Can the introduction of effective medical services for migraine improve clinical outcomes and cost-saving measures? The benefits are potentially enormous, both in terms of enhancing economic outcomes as well as addressing unmet needs in one billion people who are affected globally. As presented in this paper there are multiple key elements for improving the medical care of headache and migraine patients in Germany. Firstly, patients must receive better education about the disease and available treatment options, including the effective use of OTC drugs. This education could potentially be provided by public health-education programs. In addition, there is an ongoing need for healthcare providers (and especially GPs), to increase their respective knowledge of how to recognize, diagnose, and properly treat migraine. As such, physicians should inform themselves of and consistently adhere to recommended clinical guidelines, while educating patients on the importance of treatment adherence. Furthermore, healthcare services for patients with headache and migraine should be provided nationally in a structured, effective, and equitable manner. Finally, the development of new therapeutic options with increased effectiveness and tolerability, if adequately applied by physicians, offers targeted patients with a critical opportunity to relieve their symptoms and address ongoing challenges associated with persistent migraine.
Tables
Appendix
References
- Steiner TJ, Stovner LJ, Vos T, et al. Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain. 2018 Feb 21;19(1):17. PubMed CrossRef
- Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. 2017 Sep;390(10100):1211-1259. PubMed CrossRef
- Katsarava Z, Mania M, Lampl C, et al. Poor medical care for people with migraine in Europe – evidence from the Eurolight study. J Headache Pain. 2018 Feb 1;19(1):10. PubMed CrossRef
- Puledda F, Shields K. Non-Pharmacological Approaches for Migraine. 2018 Apr;15(2):336-345. PubMed CrossRef
- Vo P, Fang J, Bilitou A, et al. Patients’ perspective on the burden of migraine in Europe: a cross-sectional analysis of survey data in France, Germany, Italy, Spain, and the United Kingdom. J Headache Pain. 2018 Sep 10;19(1):82. PubMed CrossRef
- Bahra A. Primary Headache Disorders: Focus on Migraine. Rev Pain. 2011 Dec;5(4):2-11. PubMed CrossRef
- Goadsby PJ, Sprenger T. Current practice and future directions in the prevention and acute management of migraine. Lancet Neurol. 2010 Mar;9(3):285-98. PubMed CrossRef
- Coeytaux RR, Befus D. Role of Acupuncture in the Treatment or Prevention of Migraine, Tension-Type Headache, or Chronic Headache Disorders. 2016 Jul;56(7):1238-40. PubMed CrossRef
- Piccinni C, Cevoli s, Ronconi G, et al. A real-world study on unmet medical needs in triptan-treated migraine: Prevalence, preventive therapies and triptan use modification from a large Italian population along two years. J Headache Pain. 2019 Jun 27;20(1):74. PubMed CrossRef
- Gaul C, Diener HC, Danesch U. Improvement of migraine symptoms with a proprietary supplement containing riboflavin, magnesium and Q10: a randomized, placebo-controlled, double-blind, multicenter trial. Headache Pain. 2015;16:516. PubMed CrossRef
- Wells RE, Bertisch SM, Buettner C, et al. Complementary and alternative medicine use among adults with migraines/severe headaches. Jul-Aug 2011;51(7):1087-97. PubMed CrossRef
- WHO International Working Group for Drug Statistics Methodology, WHO Collaborating Centre for Drug Statistics Methodology & WHO Collaborating Centre for Drug Utilization Research and Clinical Pharmacological Services. Introduction to drug utilization research [Internet]. World Health Organization (2003). Date accessed: February 2, 2021. URL
- Statistisches Bundesamt. Verdienststrukturerhebung Niveau, Verteilung und Zusammensetzung der Verdienste und der Arbeitszeiten abhängiger Beschäftigungsverhältnisse – Ergebnisse für Deutschland. 2017 [Federal Statistical Office. Structure of Earnings Survey Level. Distribution and composition of earnings and of working hours in dependent employment – Results for Germany. 2017]. Date accessed February 2, 2021. URL
- Steiner TJ, Antonaci F, Jensen R,et al. Recommendations for headache service organisation and delivery in Europe. J Headache Pain. 2011 Aug;12(4):419-26. PubMed CrossRef
- Steiner TJ, Jensen R, Katsarava Z, et al. Aids to management of headache disorders in primary care (2nd edition): On behalf of the European Headache Federation and Lifting the Burden: The Global Campaign against Headache. J Headache Pain. 2019 May 21;20(1):57. PubMed CrossRef
- Diener HC, Gaul C, Kropp P. Therapie der Migräneattacke und Prophylaxe der Migräne. Nervenheilkunde. 2018;37(10):689-715. CrossRef
- Jacob L, Kostev K. Prescription Patterns and the Cost of Migraine Treatments in German General and Neurological Practices. Pain Pract. Jul;17(6):747-752. PubMed CrossRef
- Katsarava Z, Steiner TJ. Neglected headache: Ignorance, arrogance or insouciance? 2012 Oct;32(14):1019-20. PubMed CrossRef
- Radtke A, Neuhauser H. Low rate of self-awareness and medical recognition of migraine in Germany. 2012 Oct;32(14):1023-30. PubMed CrossRef
- Lucas C, Géraud G, Valade D, et al. Recognition and therapeutic management of migraine in 2004, in France: Results of FRAMIG 3, a French nationwide population-based survey. 2006 May;46(5):715-25. PubMed CrossRef
- Radtke A, Neuhauser H. Prevalence and burden of headache and migraine in Germany. 2009 Jan;49(1):79-89. PubMed CrossRef
- Cevoli S, D’Amico A, Martelletti P, et al. Underdiagnosis and undertreatment of migraine in Italy: A survey of patients attending for the first time 10 headache centres. 2009 Dec;29(12):1285-93. PubMed CrossRef
- Viana M, Khaliq F, Zecca C, et al. Poor patient awareness and frequent misdiagnosis of migraine: findings from a large transcontinental cohort. J Neurol. 2020 Mar;27(3)536-541. PubMed CrossRef
- Bösner S, Hartel S, Diederich J, Baum E. Diagnosing headache in primary care: A qualitative study of GPs’ approaches. Br J Gen Pract. 2014 Sep;64(626):e532-7. PubMed CrossRef
- Blumenfeld AM, Bloudek LM, Werner JB, et al. Patterns of use and reasons for discontinuation of prophylactic medications for episodic migraine and chronic migraine: Results from the second international burden of migraine study (IBMS-II). 2013 Apr;53(4):644-55. PubMed CrossRef
- Ahmed F, Gaul C, Garciá-Moncó JC, et al. An open-label prospective study of the real-life use of onabotulinumtoxinA for the treatment of chronic migraine: The REPOSE study. J Headache Pain. 2019 Mar 7;20(1):26. PubMed CrossRef
- Hepp Z, Dodick DW, Varon SF, et al. Persistence and switching patterns of oral migraine prophylactic medications among patients with chronic migraine: A retrospective claims analysis. 2017 Apr;37(5):470-485. PubMed CrossRef
- Linde M, Gustavsson A, Stovner LJ, et al. The cost of headache disorders in Europe: The Eurolight project. Eur J Neurol. 2012 May;19(5):703-11. PubMed CrossRef
- Bloudek LM, Stokes M, Buse DC, et al. Cost of healthcare for patients with migraine in five European countries: results from the International Burden of Migraine Study (IBMS). J Headache Pain. 2012 Jul;13(5):361-78. PubMed CrossRef
- Porter JK, Di Tanna GL, Lipton RB, et al. Costs of Acute Headache Medication Use and Productivity Losses Among Patients with Migraine: Insights from Three Randomized Controlled Trials. Pharmacoecon Open. 2019 Sep;3(3):411-417. PubMed CrossRef
Disclosures
Conflicts of interest and Funding statement: This study was financially supported by AbbVie GmbH. Alice Eberhardt and Tim Kirchmann are employees of AbbVie GmbH. Fränce Hardtstock and Zeki Kocaata are employees of Ingress-Health and have no conflict of interest to declare. Thomas Wilke, who is the managing director of IPAM e.V., has worked as a consultant for Boehringer Ingelheim Pharma, Bayer Health Care, GSK, Novartis, Sanofi-Aventis, Bristol Myers Squibb, Pfizer and other pharmaceutical companies. Ulf Maywald works for one of the insurance funds that provided the study data (AOK PLUS). Zaza Katsarava is a Director and Trustee of ‘Lifting The Burden’ and the ‘European Headache Federation’ and has supported the study as a scientific advisor. Otherwise, he does not declare a conflict of interest.
