Author: Ian C Holmen MD * 1, Justin Merkow MD 1, Jennifer Kummer MD 2, Narayana Varhabhatla MD 1
Author Affiliation:
1 Department of Anesthesiology, University of Colorado Hospital, Aurora, CO, USA
2 Department of Orthopedic Surgery, University of Colorado Health Steadman Hawkins Clinic Denver, Englewood, CO, USA
Competing Interests: The author/s declare no competing interests.
Issue: 04.05
DOI: 10.30756/ahmj.2020.04.05
Received: Dec 30, 2020
Revised: Mar 4, 2021
Accepted: Mar 5, 2021
Published: March 16, 2021
Recommended Citation: Holmen IC, Merkow J, Kummer J, Varhabhatla N. A Case of Successful Treatment of Iatrogenic Superficial Cervical Plexus Neuropathy Following Upper Extremity Surgery with Interscalene Brachial Plexus Block. Ann Head Med. 2020;04:05. DOI: 10.30756/ahmj.2020.04.05
Objectives
To describe the successful treatment for iatrogenic superficial cervical plexus neuropathy following brachial plexus block, which is a rare complication of this procedure.
Case Report
We present a case report of a 67-year-old male who underwent a surgical excision of gouty tophi of the thumb and index finger with brachial plexus block for postoperative pain control. He had no prior history of chronic headaches or facial neuropathic pain. Thirty-six hours following surgery the patient experienced burning pain in his occiput, jaw, ear, and proximal shoulder. The patient was diagnosed with iatrogenic superficial cervical plexus neuropathy, which proved refractory to oral methylprednisolone and neuropathic medications. A superficial cervical plexus injection with bupivacaine and dexamethasone resulted in an 80% resolution of pain for over 6 months.
Conclusion
Superficial cervical plexus injury may occur following interscalene brachial plexus nerve block. Superficial cervical plexus block may provide early effective treatment for neuropathy refractory to conservative measures.
Introduction
The brachial plexus block is widely used for patients undergoing shoulder and upper extremity surgery. Complications due to regional anesthetic technique have been well documented in the literature and generally include paresthesia, dysesthesia, and pain unrelated to surgery.1, 2, 3, 4 Specifically for the interscalene approach, both brachial plexus injury and damage to the four cutaneous branches of the superficial cervical plexus have been reported.2, 5 Christ et al. observed that up to 7.7% of patients receiving an interscalene block for shoulder or upper arm surgery experienced hyperesthesia in the area of distribution of the superficial cervical plexus prior to standard use of ultrasound.5
The cervical plexus block is traditionally used for head and neck surgeries and is most commonly used for carotid endarterectomies.6 The superficial branches of the cervical plexus originate from C2-C4 and form the lesser occipital, great auricular, transverse cervical, and supraclavicular sensory branches. These branches initially run deep to the prevertebral fascia in a groove between the longus capitis and the middle scalene muscles but not in the interscalene groove. The branches then pierce the prevertebral fascial and travel through the interfacial space between the sternocleidomastoid muscle and the prevertebral muscles before reaching their superficial structures. Blocking the superficial plexus nerves allow for analgesia in certain surgeries such as thyroidectomies and has even been effective as the sole anesthetic modality for external ear surgery.7
While iatrogenic injury to the superficial cervical plexus following interscalene brachial plexus block has been described, to our knowledge there have been no reports of successful treatment of this neuropathy with a superficial cervical plexus steroid injection. It is not intuitively obvious that iatrogenic injury to a nerve should be treated with another injection, as both provider and patient would be appropriately anxious about exacerbating the existing injury.
Case Report
We report on a 67-year-old male with a history of hypertension, arthritis, and multiple gouty tophi of his left hand involving the interphalangeal joints of the thumb and index finger who underwent surgical excision for improvement in motion and pain control. He had no prior history of migraine, jaw pain, intractable headaches, or pain of the face. He had no prior trauma, operations of the head or neck. He worked as a salesperson and used the phone frequently but reported no history of face pain or headaches with his job.
Pre-operatively, the patient received an interscalene brachial plexus block for postoperative pain control. The patient received 1 mg midazolam for sedation prior to the nerve block. The patient was positioned with the head of the bed at 30 degrees and the brachial plexus was identified in the supraclavicular fossa under ultrasound and traced up between the supraclavicular fossa and the interscalene groove. A 4-inch, 21-gauge Stimuplex needle (B. Braun Medical Inc., Bethlehem, PA) with a 30° back-cut bevel was then inserted from the posterior lateral side in-plane to the ultrasound beam. Thirty milliliters of 0.5% ropivacaine were then deposited around the brachial plexus. The patient tolerated the procedure well and there was no resistance, pain, or paresthesia on injection. There is no documentation of the patient reporting a headache or radiating pain to the head or jaw during the injection.
The surgery was completed successfully under sedation without any complications. During surgery the patient was in the supine position with the operative arm abducted at less than 90 degrees. Following surgery, the patient reported good pain control and was discharged home from the post-anesthesia care unit. Thirteen days after surgery the patient returned for routine surgical follow up and reported left sided facial pain that had begun 36-48 hours after surgery. He reported the pain as nine out of ten for severity and burning in nature. This pain had not improved with self-medication with Tylenol or ibuprofen. The facial pain and headache had persisted while the pain in his hand had fully resolved with participation in physical therapy. He denied photophobia, phonophobia, nausea, recent rash on face or head, exposure to herpes zoster, or use of over-the-counter analgesics on a regular basis. He was then referred to our pain clinic for further evaluation.
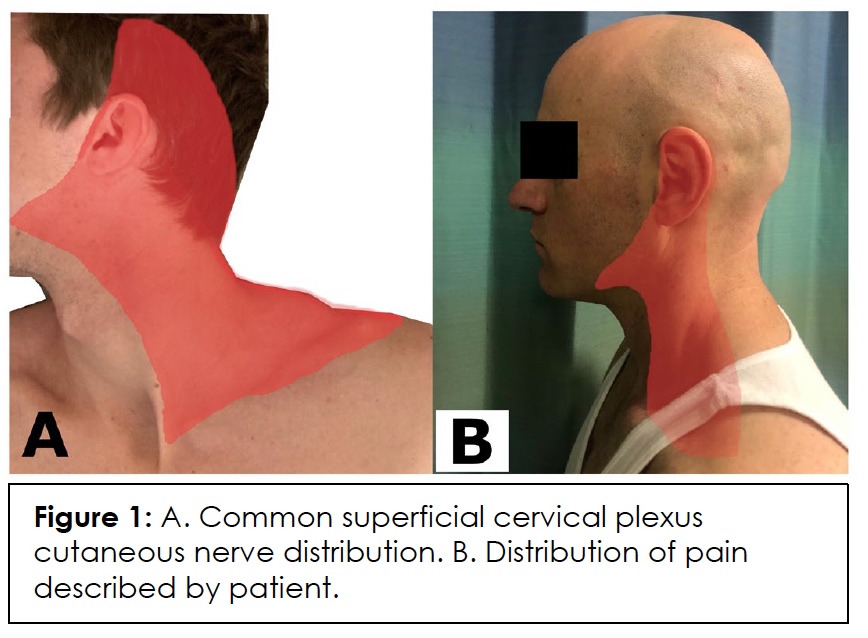
On postoperative day (POD) 20, the patient was seen in the pain clinic where he reported continuous and debilitating burning pain in his left occiput, bottom of the jaw to the chin and to the left ear (Figure 1). He reported difficulty eating and speaking and denied having similar pain the past or rashes in the area of distribution. He had tried acupuncture and chiropractor treatments and was taking 800mg ibuprofen once daily without relief of facial pain. He was then given a presumptive diagnosis of iatrogenic superficial cervical plexus neuropathy. He was prescribed methylprednisolone 4mg TID for 7 days and gabapentin 300mg TID. The pain persisted and the patient was offered a diagnostic superficial cervical plexus block.
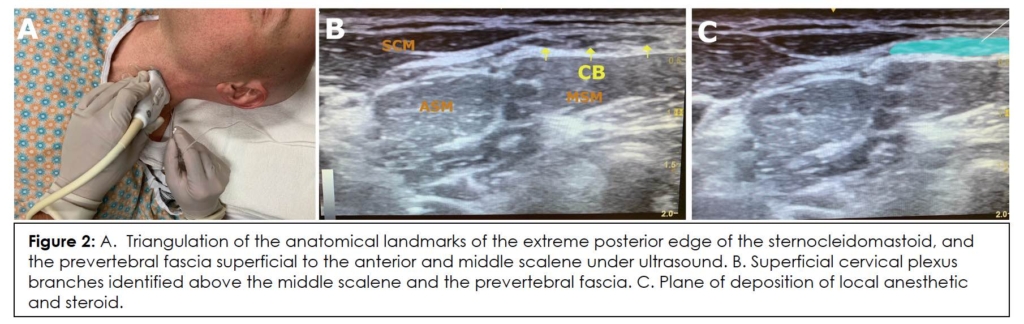
On POD 49 the patient returned to pain clinic reporting no improvement in the intensity, quality, or distribution of his pain. He wished to proceed with a superficial cervical plexus injection, after extensive discussion about the possible risk of further iatrogenic injury during the injection itself. The superficial cervical plexus was located under ultrasound guidance using the anatomical landmarks of the extreme posterior edge of the sternocleidomastoid, and the superficial layer of the deep cervical fascia superficial to the anterior and middle scalene at the intervening portion of the brachial plexus roots (Figure 2). The site was prepped and draped in a sterile fashion. A 27 gauge, 1.5-inch needle was inserted in plane under direct ultrasound visualization and 4ml of 0.5% bupivacaine with 4mg dexamethasone were injected around the superficial cervical plexus. The patient reported greater than 50% improvement in pain within the first 30 minutes of injection. On POD 64 the patient was contacted by phone and reported 80% improvement in pain and reported that the majority of the improvement occurred at 2 weeks following the steroid injection.
Discussion
We report a case of superficial cervical plexus neuropathy after a surgical brachial plexus block that responded well following a superficial cervical plexus block with local anesthetic and dexamethasone. There is an intuitive concern about injecting a plexus that is already irritated may exacerbate the pain. However, previous reports of similar methods have been utilized in post-injection sciatic neuropathy (PISN). One report by Eker et al. described five patients who experienced severe neuropathic pain and weakness secondary to gluteal intramuscular injections. All patients had good response to diagnostic nerve blocks with lidocaine deposited through the sacral foramina and then experienced complete recovery following an 80mg perineural injection of methylprednisolone.8 Similarly, Sencan et al. report 3 cases of PISN pain refractory to conventional treatments and physiotherapy that improved following similar methylprednisolone injections with using a fluoroscopy-guided transforamenal transsacral block.9
The risk of direct injury to the superficial cervical plexus is possible given the site of the needle insertion for an interscalene block. The superficial sensory branches of the cervical plexus traverse over the middle scalene muscle after piercing the prevertebral fascia and are noted in Figure 2B and consequently direct mechanical injury to these nerves from the posterior lateral approach is possible. The distribution of the patient’s pain appears to coincide with multiple superficial branches of the superficial plexus, which may have been caused by needle insertion. While not reported in this case, it is possible that skin infiltration with local anesthetic using a sharp needle prior to an interscalene block may also risk damage to the superficial cervical plexus.
To our knowledge, this is the first report of superficial cervical plexus injury from an interscalene brachial plexus nerve block in the last decade in which the use of ultrasound has become standard. Prior to ultrasound being the standard of care, Christ et al. followed 273 patients who underwent interscalene brachial plexus block and followed them for 6 months. They report a 7.7% incidence of superficial cervical plexus neuropathy with 1.8% of patients having symptoms for more than 31 days. All patients had resolution of symptoms in 6 months. However, there have been reports of nerve injury lasting for up to one year.5,10 This patient reported no symptoms of brachial plexus injury and had resolution of his numbness in the upper extremity. Our hypothesis is that this was a direct needle injury of the superficial cervical plexus itself. The patient likely did not perceive pain immediately given the volume of local anesthetic that may have traveled cephalad, blocking conduction proximal to the site of injury. Research on nerve damage resulting from crush injuries suggest that dexamethasone and methylprednisolone may accelerate nerve recovery through reducing oxygen radicals and lipid peroxidation.11, 12 Moreover some data suggest that the use of local steroids may be more effective than their systemic application in nerve recovery.13
This single case report has multiple limitations. The injection of steroid could have been therapeutic in and of itself. Ideally, we would have done a single diagnostic local-only injection to confirm diagnosis, and then a steroid injection if needed for therapeutic response. Christ et al. note that 76% of patients have resolution of symptoms before 31 days, so it’s possible that his injury and pain would have resolved on its own without intervention. Practically, this patient was a busy salesman, and this pain was debilitating so he needed quick resolution in order to function at work and maintain his livelihood. However, we think that early diagnosis can lead to potential resolution with a simple intervention.
Overall, this case demonstrates the possible use of superficial cervical plexus steroid injections for the treatment of post-brachial plexus block superficial cervical plexus neuropathy. We hope this case report will alert the reader to this potential complication of the common interscalene brachial plexus block and review the anatomy of the cervical plexus and its blockade.
References
- Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007 Apr;104(4):965-74. PubMed CrossRef
- Candido KD, Sukhani R, Doty R Jr, Nader A, et al. Neurologic sequelae after interscalene brachial plexus block for shoulder/upper arm surgery: the association of patient, anesthetic, and surgical factors to the incidence and clinical course. Anesth Analg. 2005 May;100(5):1489-95. PubMed CrossRef
- Fanelli G, Casati A, Garancini P, Torri G. Nerve stimulator and multiple injection technique for upper and lower limb blockade: failure rate, patient acceptance, and neurologic complications. Study Group on Regional Anesthesia. Anesth Analg. 1999 Apr;88(4):847-52. PubMed CrossRef
- Selander D, Dhuner KG, Lundborg G. Peripheral nerve injury due to injection needles used for regional anesthesia. An experimental study of the acute effects of needle point trauma. Acta Anaesthesiol Scand. 1977;21(3):182-8. PubMed CrossRef
- Christ S, Rindfleisch F, Friederich P. Superficial Cervical Plexus Neuropathy after Single-Injection Interscalene Brachial Plexus Block. Anesth Analg. 2009 Dec;109(6):2008-11. PubMed CrossRef
- Martusevicius R, Swiatek F, Joergensen LG, Nielsen HB. Ultrasound-guided locoregional anesthesia for carotid endarterectomy: A prospective observational study. Eur J Vasc Endovasc Surg. 2012 Jul;44(1):27-30. PubMed CrossRef
- Ritchie MK, Wilson CA, Grose BW, et al. Ultrasound-guided greater auricular nerve block as sole anesthetic for ear surgery. Clin Pract. 2016 May 23;6(2):856. PubMed CrossRef
- Eker HE, Cok OY, Aribogan A. A treatment option for post-injection sciatic neuropathy: transsacral block with methylprednisolone. Pain Physician. Sep-Oct 2010;13(5):451-6. PubMed
- Şencan S, Cüce I, Gündüz OH. Use of fluoroscopic-guided transsacral block for the treatment of iatrogenic post-injection sciatic neuropathy: Report of three cases. Turk J Phys Med Rehabil. 2019 Nov;65(4):406-410. PubMed CrossRef
- Fredrickson MJ. Superficial Cervical Plexus Neuropathy with Chronic Pain After Superficial Cervical Plexus Block and Interscalene Catheter Placement. Reg Anesth Pain Med. Mar-Apr 2011;36(2):206. PubMed CrossRef
- Feng, X. & Yuan, W. Dexamethasone enhanced functional recovery after sciatic nerve crush injury in rats. Biomed Res Int. 2015;2015:627923. PubMed CrossRef
- Nachemson AK, Lundborg G, Myrhage R, Rank F. Nerve regeneration and pharmacological suppression of scar reaction at the suture site: An experimental study on the effect of estrogen-progesterone, methylprednisolone-acetate and cis-hydroxyproline in rate sciatic nerve. Scand J Plast Reconstr Surg. 1985;19(3):255-260. PubMed CrossRef
- Suslu H, Altun M, Erdivanli B, Turan SH. Comparison of the effects of local and systemic dexamethasone on the rat traumatic sciatic nerve model. Turk Neurosurg. 2013;23(5):623-629. PubMed CrossRef
Disclosures
Consent/Permissions: Patient consent was received to report the case.
Funding: No sources of funding.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
