Author: Leith Andrew Hobbs* DO 1, Kimberley Haynes-Henson MD 2
Author Affiliation:
1 PGY-III Neurology Resident, University of Nebraska Medical Center, Omaha, Nebraska
2 Associate Professor of Anesthesiology, University of Nebraska Medical Center, Omaha, Nebraska
Competing Interests: The author/s declare no competing interests.
Issue: 09.01
DOI: 10.30756/ahmj.2022.09.01
Received: Sept 19, 2022
Revised: Nov 7, 2022
Accepted: Nov 11, 2022
Published: Nov 29, 2022
Recommended Citation: Hobbs L, Haynes-Henson K. A Case Of Probable Paroxysmal Hemicrania Mistaken For Cervicogenic Headache. Ann Head Med. 2022;09:01. DOI: 10.30756/ahmj.2022.09.01
Objectives: To describe a unique case of probable paroxysmal hemicrania which was mistaken for cervicogenic headache and to investigate reasons for misdiagnosis, which includes imperfect diagnostic criteria, unique pathophysiology, and inadequate headache education in the field of pain medicine.
Case report: We present a sixty-six-year-old female with multiple disorders of the cervical spine and a two-year history of left-sided neck pain and headache. She was seen by multiple specialists and originally assumed to have cervicogenic headache. She did not respond to conservative measures or medial branch block. Ultimately, she was suspected to have paroxysmal hemicrania, despite her not having obvious autonomic features. She obtained complete relief with indomethacin.
Conclusions: Trigeminal autonomic cephalalgias such as paroxysmal hemicrania and hemicrania continua can be mistaken for cervicogenic headache. The diagnostic criteria for cervicogenic headache should be better defined. Cervicogenic headache and the trigeminal autonomic cephalalgias, including paroxysmal hemicrania, can refer pain to various areas of the head and neck.1-4 This occurs via convergent afferent fibers and the trigeminocervical complex. 5-7 This overlapping symptomatology and pathophysiology explains how misdiagnosis of certain headache disorders can occur. Lastly, it is imperative that pain medicine providers have adequate training in headache medicine.
Introduction
Cervicogenic headache (CEH) is a common condition seen in pain clinics. The trigeminal autonomic cephalgias (TACs), such as paroxysmal hemicrania (PH), are less common. There is limited evidence in the literature that describes PH being mistaken for CEH. We report a unique case of probable PH that mimicked CEH. We investigate the factors which contributed to this misdiagnosis. This case demonstrates that TACs can cause pain outside the distribution of the trigeminal nerve. It also reveals that the diagnostic criteria for CEH is imperfect. Lastly, this case highlights the importance of headache education among pain medicine trainees.
Case Report
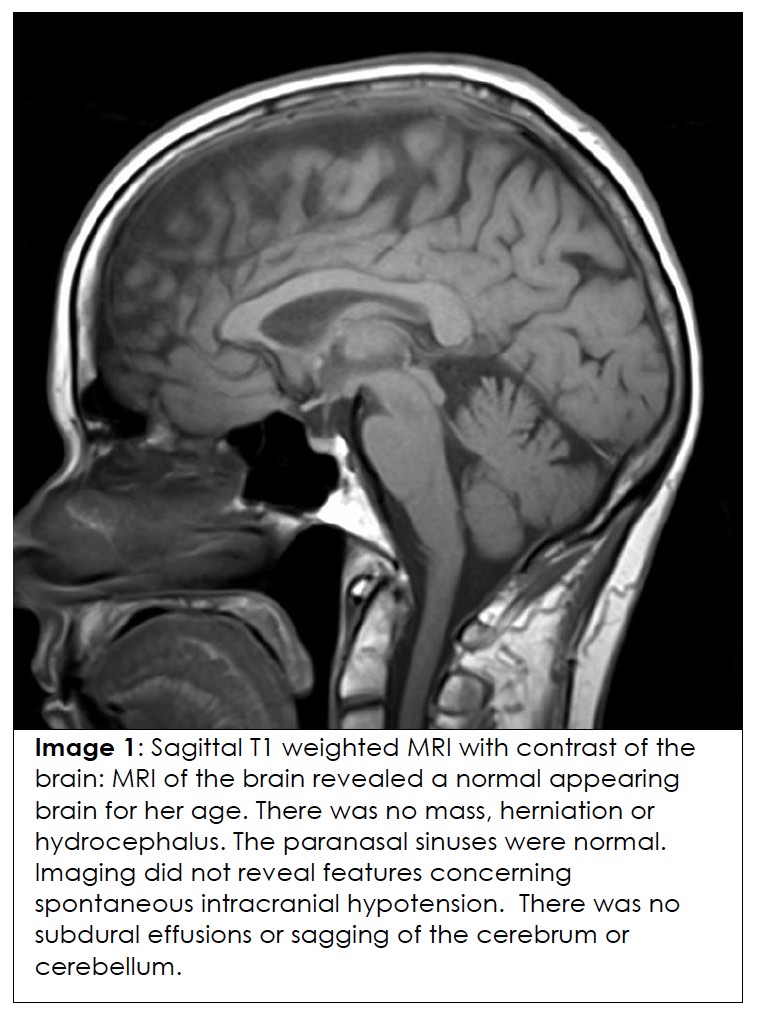
Our case describes a 66-year-old female with cervical spondylosis and a history of a collision injury while ice-skating in 2019. In spring of 2020 she began experiencing left-sided neck pain and headache. She reported experiencing sharp pain starting in the left lateral and posterior cervical region which radiated to the left temporal and frontal region and occurred intermittently throughout the day. Her symptoms were provoked by sitting and often alleviated when laying down. At times, a sense of disequilibrium accompanied her pain. She was originally evaluated by her primary doctor, a neuro-otologist, physical therapist, and a physiatrist. She did not respond to acetaminophen, sumatriptan, or methylprednisolone. She also did not respond significantly to nonsteroidal anti-inflammatory drugs, including a several week-long trial of naproxen dosed at 220 mg twice daily and an additional three week trial of meloxicam 7.5mg taken daily. She did not improve with physical therapy. Magnetic resonance imaging (MRI) of the brain (image 1) was unremarkable and did not reveal features concerning for spontaneous intracranial hypotension. 8 Her MRI imaging did not reveal dural or pachymeningeal contrast enhancement, subdural effusions, or downward sagging of the cerebrum or cerebellum.
Her physical therapist and physiatrist noticed that she had mildly restricted range of motion in the cervical spine, particularly with leftward side-bending and rightward rotation. Upon palpation they noticed she had hypertonicity of the upper thoracic musculature. The patient’s physiatrist diagnosed her with cervicogenic headache and referred her to a pain physician.
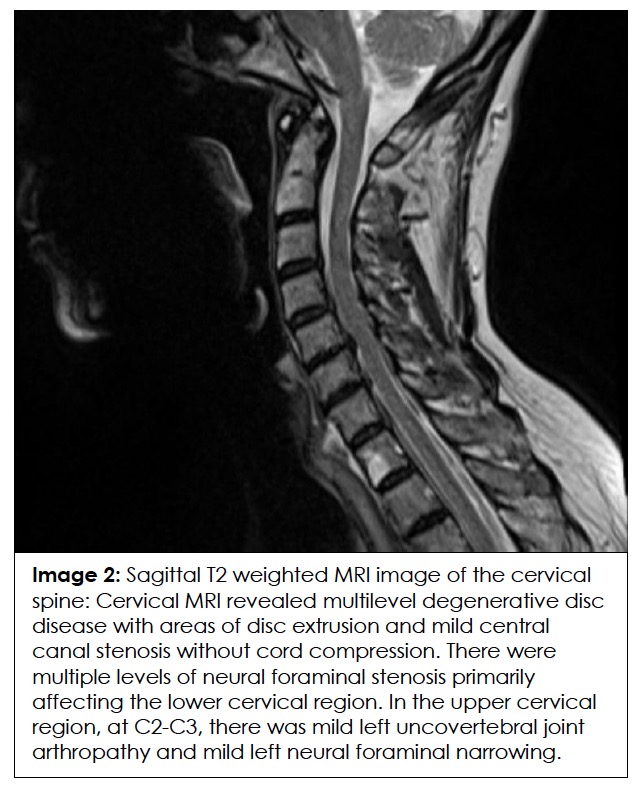
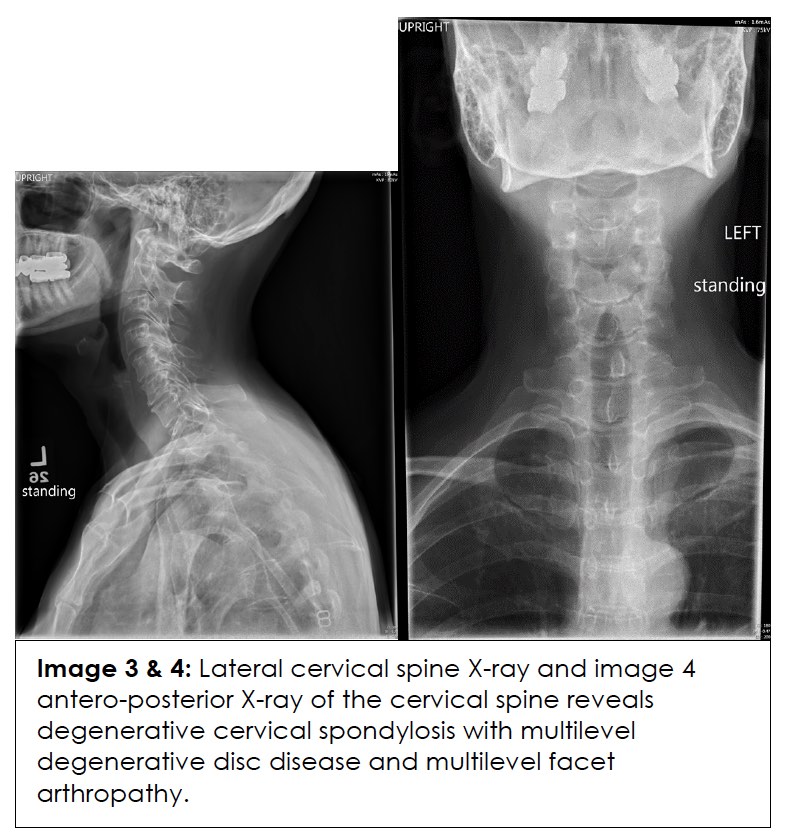
Her pain physician agreed with the diagnosis of CEH and ordered an MRI of the cervical spine (image 2) which showed evidence of degenerative disc disease, central canal stenosis without cord compression, facet arthropathy, and neural foraminal stenosis at multiple levels bilaterally. Specifically, there was mild left uncovertebral joint arthropathy and mild left neural foraminal narrowing at the C2-C3 level. At C3-C4 there was mild facet arthropathy bilaterally, with mild left and moderate right neural foraminal stenosis. At C4-C5 there was loss of disc height, in addition to uncovertebral and facet joint arthropathy. Also, at C4-C5 there was severe bilateral neural foraminal stenosis with impingement of the left C5 nerve root. Likewise, at the C5-C6, C6-C7, and C7-T1 levels there was degenerative disc disease, facet arthropathy and neural foraminal stenosis throughout with bilateral impingement of the C6 nerve roots and abutment of the left C7 nerve root. Images 3 and 4 reveal our patient’s cervical spine X-rays taken 1 month prior, which show similar spondylitic and degenerative features.
In March of 2022, her pain physician performed a block of the left C3, C4, C5 medial branches, and the left third occipital nerve using 0.5% bupivacaine. No benefit was achieved. Weeks later she presented to our emergency department. Basic labs and computed tomography angiography (CTA) of the head and neck were unremarkable. Our neurology service was consulted. That night she described her headaches as being a sharp pain, nine out of ten in severity, affecting the left temporal, occipital, and posterior upper cervical region. The attacks lasted up to thirty minutes, then remitted entirely, reoccurring every one to two hours. She did not experience a headache in between the paroxysms of pain. She reported having more than ten occurrences a day and being woken up by the attacks at night. She denied numbness, tingling, visual disturbances, aura, or a sense of restlessness during the attacks. It was not associated with autonomic signs. She confirmed that these headaches were the same symptoms she had experienced over the past year. Her neurological exam was unremarkable and was without obvious autonomic irregularities. However, at the time of her neurological examination she was not experiencing a paroxysm of pain, as the intermittent pain had subsided an hour prior.
Since she did not report autonomic symptoms and lacked autonomic findings on examination, she best fit the diagnosis of probable paroxysmal hemicrania at that time. She was then started on indomethacin. At her two-month follow-up she reported complete relief with twenty-five milligrams twice daily. However, anytime she misses a dose her attacks reoccur.
Discussion
Several factors led to the delay in this patient obtaining an accurate diagnosis and treatment. These factors include the complex pathophysiology and semiology of this type of headache, difficulty utilizing diagnostic criteria, and lack of headache education for pain medicine trainees.
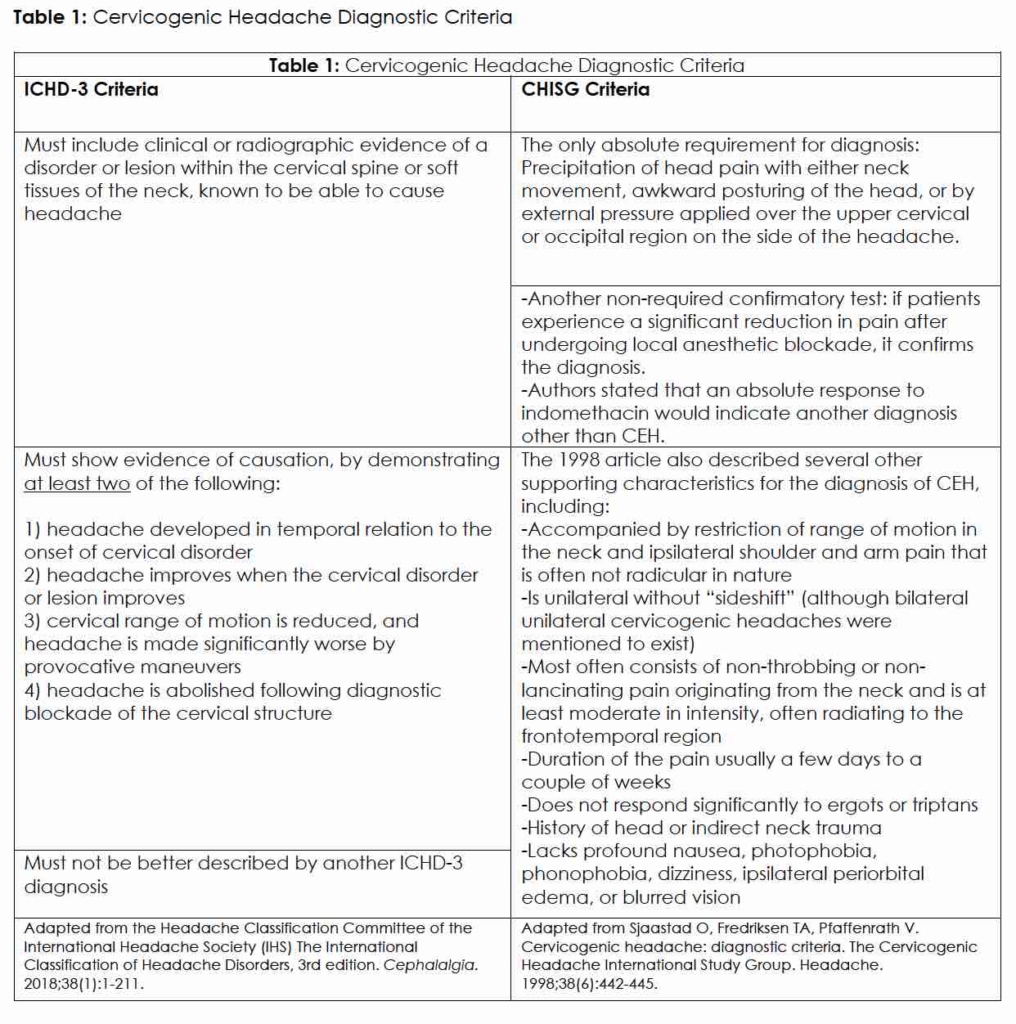
CEH is one of the most common types of headaches, with an estimated incidence worldwide of 2-4%. It represents 25% of all headaches encountered in pain clinics. 6 The International Headache Society (IHS) defines cervicogenic headache as a “headache caused by a disorder of the cervical spine and its component bony, disc, and/or soft tissue elements, usually but not invariably accompanied by neck pain.” There are two main diagnostic criteria for the diagnosis of CEH, which include the IHS International Classification of Headache Disorders-III (ICHD-3) criteria and the Cervicogenic Headache International Study Group (CHISG) criteria. ICHD-3 is more recent and the CHISG criteria was last revised in 1998. 9, 10 (Table 1 compares the two.)
The ICHD-3 diagnostic criteria has components that some clinicians feel are difficult to utilize in practice. These critics state that it is unrealistic to determine if head pain develops in temporal relation to a cervical disorder, as these conditions develop very slowly. 11 The CHISG criteria, which was last revised and published in Headache in 1998, provided a deeper explanation of cervicogenic headache. However, it offered less absolute diagnostic criteria and was confusing.
When comparing the initial patient presentation to these diagnostic tools, you can see how pain medicine clinicians with limited training in headache medicine could potentially diagnose this as cervicogenic headache. She had side-locked headache ipsilateral to her neck pain, degenerative and arthritic changes on radiography, restricted range of motion in the neck, a history of injury, and symptoms which worsened upon certain position changes.
According to Narouze, the anatomical sources of cervicogenic headache involve structures innervated by the upper three cervical spinal nerves, which would include the atlantooccipital joint, atlantoaxial joint, C2-C3 intervertebral disk, C2-C3 facet joint, in addition to musculature in the upper posterior cervical and paravertebral musculature. Abnormalities in the trapezius, sternocleidomastoid muscle, posterior cranial fossa dura mater, or upper cervical nerve roots have also been implicated in CEH. 12 In our patient, the only radiographic findings that potentially meet this component of the criteria would be the mild left-sided uncovertebral joint arthropathy and mild left neural foraminal narrowing at C2-C3. The mild restricted range of motion she had in the neck and the hypertonicity she experienced in the upper left portion of the trapezius may also add supporting evidence for this being CEH.
Prior to the negative response to diagnostic block and the positive indomethacin response, the patient did meet some criteria for CEH according to the CHISG and the ICHD-3 criteria. 9, 10 The initial misdiagnosis of cervicogenic headache in this case exemplifies the challenge clinicians have making this diagnosis. There have been high rates of misdiagnosis of CEH in the past, with reported rates varying from 50% to 92.45%. 13 Some novice clinicians may inappropriately think that all headaches with neck pain must be cervicogenic headache.
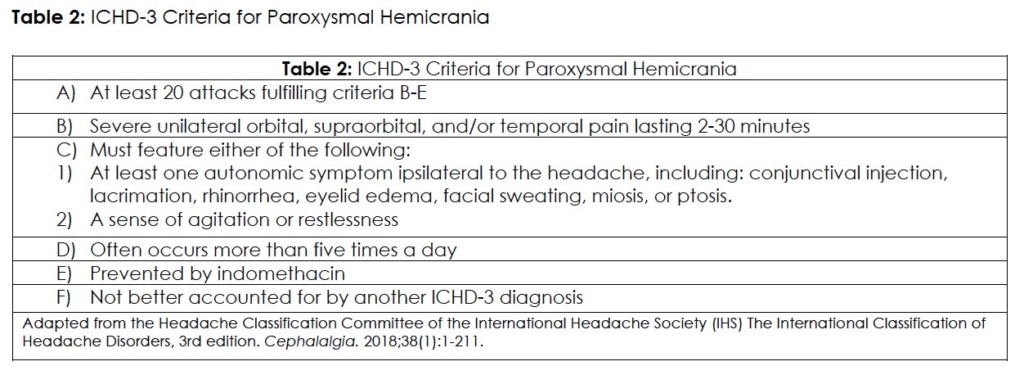
The patient eventually was suspected to have PH, which was further supported by her exquisite response to indomethacin. The ICHD-3 diagnostic criteria for PH are described in Table 2.
Another challenging aspect to this case was that our patient denied experiencing any of the classic autonomic symptoms and lacked noticeable autonomic features on physical exam during her neurological consultation. Technically, our patient only meets ICHD-3 criteria for probable paroxysmal hemicrania.9 However, one could hypothesize that when not taking the indomethacin our patient could experience some subtle cranial parasympathetic changes that would be capturable on examination, that were simply not apparent during her initial neurological consultation. As previously stated, our neurology service was unable to examine the patient during the time of one of her paroxysms of pain and thus may have missed transient autonomic related exam findings.
Although not a component in the ICHD-3 criteria, there are several reports of PH attacks being accompanied by neck pain or being provoked by neck movements. 1-4 10% of patients can trigger attacks with neck movements.1 One small prospective trial reported neck pain accompanying paroxysmal hemicrania attacks in eight of thirty-one patients.2 It is easy for clinicians to forget that PH attacks can be accompanied by referred pain to the neck. Thus, a proper understanding of the underlying pathophysiology is important.
TACs can be associated with pain outside of the trigeminal nerve distribution. They frequently refer pain to the occipital and cervical regions. This phenomenon occurs because of convergence of cervical, meningeal, and trigeminal nociceptive afferent fibers to the trigeminocervical complex and its relay to the brain stem and higher brain centers.3, 5, 7 A similar mechanism is used to describe the pathophysiology of cervicogenic headache,6 which explains why several of these conditions can mimic each other.
Another differentiating factor between hemicrania continua, PH, and CEH is their varying responsiveness to indomethacin. Hemicrania continua and PH respond absolutely to indomethacin. With CEH, you would not expect such a dramatic response to low dose indomethacin and a negligible response to other non-steroidal anti-inflammatory drugs. Indomethacin differs from other cyclooxygenase inhibitors as it penetrates the blood-brain barrier at higher rates, reduces intracranial pressure, and exhibits unique effects on the hypothalamus and autonomic system. 14 Indomethacin also has exceptional effects on the nitric oxide system which may be of particular importance to PH. PH attacks have been shown to be induced by the nitric oxide donor glyceryl trinitrate and subsequently reversed by indomethacin.15
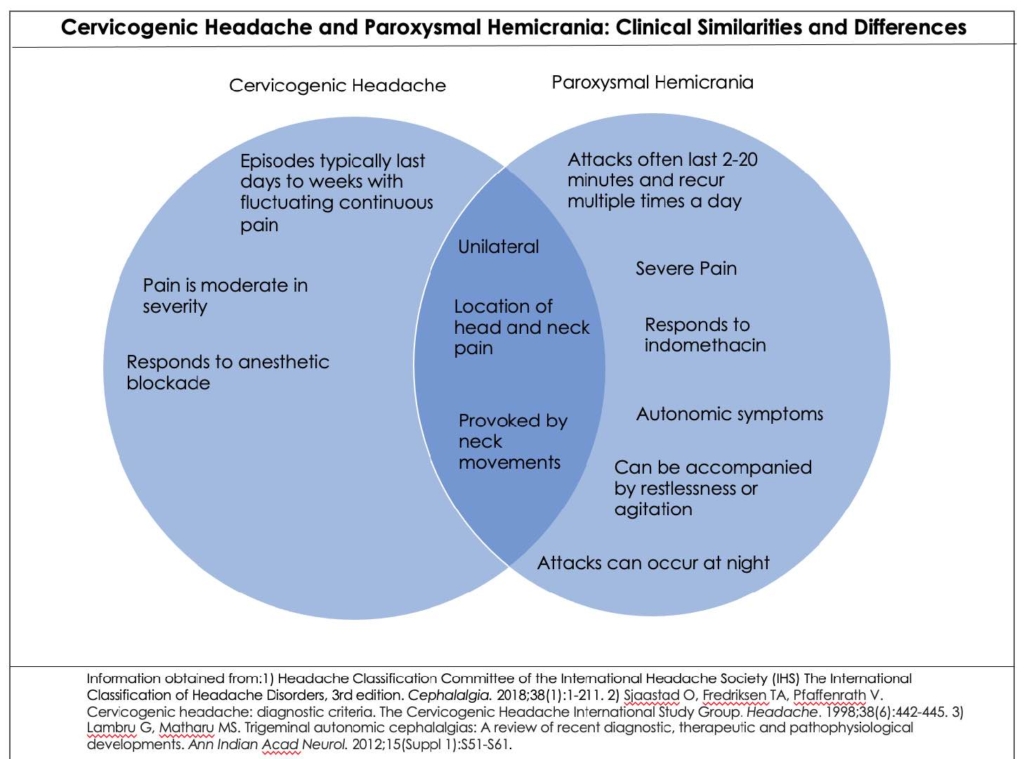
The diagnosis of PH for our case was suspected due to the short duration, frequency of the attacks, indomethacin responsiveness, and the quality of her pain. Also, admittedly, our neurology service had the advantage of a failed medial branch block to eliminate CEH from our differential. In summary, the figure below describes ways to differentiate between CEH and PH.
It is likely that CEH or a CEH mimic would present to a pain clinic. Pain medicine providers should be well educated in the field of headache medicine to provide appropriate treatment and not perform unnecessary procedures.
Although headache is a common complaint to pain clinics, headache medicine education is often lacking in certain ACGME pain fellowships. In one survey, approximately 25% of pain fellowship program directors (PDs) indicated that their fellows received “minimal” to “no” training on medication overuse headache, trigeminal autonomic cephalgias, and migraine specific medications. 50% of PDs also reported that pain fellows received little to no education on interventional headache procedures. Surprisingly, 66% of PDs reported that they did not have a board-certified headache specialist on staff.16 This lack of training could certainly lead to diagnostic and therapeutic errors.
Conclusion
This case demonstrates that TACs, such as PH, can be mistaken for CEH. The TACs can refer pain to the neck via convergent afferent fibers and the activity of the trigeminocervical complex. CEH is a diagnosis of exclusion and a condition that needs to be better defined in literature. Although specific guidelines for headache disorders exist, it is often clinical experience that overcomes shortcomings in diagnostic literature. Lastly, pain medicine providers must have adequate training in headache medicine.
Tables
References
- Boes C VM, Russell D. Paroxysmal Hemicrania. In: Olesen J GP, Ramadan N, Tfelt-Hansen P, Welch K, ed. The Headaches. Lippincott Williams & Wilkins; 2005.
- Cittadini E, Matharu MS, Goadsby PJ. Paroxysmal hemicrania: a prospective clinical study of 31 cases. Brain. Apr 2008;131(Pt 4):1142-55. PubMed PMID: 18252775. doi:10.1093/brain/awn010
- Lambru G, Matharu MS. Trigeminal autonomic cephalalgias: A review of recent diagnostic, therapeutic and pathophysiological developments. Ann Indian Acad Neurol. Aug 2012;15(Suppl 1):S51-61. PubMed PMID: 23024564; PubMed Central PMCID: PMCPMC3444219. doi:10.4103/0972-2327.100007
- Viana M, Tassorelli C, Allena M, Nappi G, Sjaastad O, Antonaci F. Diagnostic and therapeutic errors in trigeminal autonomic cephalalgias and hemicrania continua: a systematic review. J Headache Pain. Feb 18 2013;14:14. PubMed PMID: 23565739; PubMed Central PMCID: PMCPMC3620440. doi:10.1186/1129-2377-14-14
- Basedau H, Nielsen T, Asmussen K, et al. Experimental evidence of a functional relationship within the brainstem trigeminocervical complex in humans. Pain. Apr 1 2022;163(4):729-734. PubMed PMID: 34326294. doi:10.1097/j.pain.0000000000002417
- Edwards L-A HL, Agarwal D, Khan D, Tolba R. Cervicogenic Headache. In: Benzon H RJ, Wu C, et al., ed. Practical Management of Pain. Elsevier; 2022:545-549.
- Piovesan EJ, Kowacs PA, Oshinsky ML. Convergence of cervical and trigeminal sensory afferents. Curr Pain Headache Rep. Oct 2003;7(5):377-83. PubMed PMID: 12946291. doi:10.1007/s11916-003-0037-x
- Ropper A SM, Klein J, Prasad S. Disturbances of Cerebrospinal Fluid, Including Hydrocephalus, Pseudotumor Cerebri, and Low-Pressure Syndromes. In: Neurology AaVsPo, ed. Adams and Victor’s Principles of Neurology. McGraw-Hill; 2019:654-656:chap 29.
- Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. Jan 2018;38(1):1-211. PubMed PMID: 29368949. doi:10.1177/0333102417738202
- Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. The Cervicogenic Headache International Study Group. Headache. Jun 1998;38(6):442-5. PubMed PMID: 9664748. doi:10.1046/j.1526-4610.1998.3806442.x
- Fredriksen TA, Antonaci F, Sjaastad O. Cervicogenic headache: too important to be left un-diagnosed. J Headache Pain. 2015;16:6. PubMed PMID: 25604994; PubMed Central PMCID: PMCPMC4417107. doi:10.1186/1129-2377-16-6
- Narouze S. Practical Approach to Cervicogenic Headache. In: Narouze S, ed. Interventional Management of Head and Face Pain: Nerve Blocks and Beyond. Springer; 2016:67-72.
- Bonakdar Tehrani M A AM, Dadgoo M. Misdiagnosis of Patients with Cervicogenic Headache: A Case Series Study. Func Disabil J. 2018;1(4):54-61. doi:10.30699/fdisj.1.4.54
- Burish MJ, Rozen TD. Trigeminal Autonomic Cephalalgias. Neurol Clin. Nov 2019;37(4):847-869. PubMed PMID: 31563236. doi:10.1016/j.ncl.2019.07.001
- Villar-Martinez MD, Moreno-Ajona D, Chan C, Goadsby PJ. Indomethacin-responsive headaches-A narrative review. Headache. May 2021;61(5):700-714. PubMed PMID: 34105154. doi:10.1111/head.14111
- Kohan L, Narouze S, Souza D, et al. Do Pain Medicine Fellowships Provide Adequate Education in Head and Facial Pain? A Survey of Pain Medicine Fellowship Program Directors. Ann Head Med. April 21, 2020 2020;2(5). doi:10.30756/ahmj.2020.02.05
Declarations/Disclosures
Consent/Permissions: The patient approved reporting of this case.
Funding: None.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, author declares the following:
Payment/services info: Author has declared that no financial support was received from any organization for the submitted work.
Financial relationships: Author have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: Author have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
