Author: Patrick M. Chen* 1, Sharona Ben-Haim 2, Jason Handwerker 3, Hossein Ansari 1
Author Affiliation:
1 Department of Neurosciences, University of California, San Diego
2 Department of Neurosurgery, University of California, San Diego
3 Department of Radiology, University of California, San Diego
Research Support: Support was provided solely from institutional and/or departmental sources.
Competing Interests: The author/s declare no competing interest
Issue: 01.02
DOI: doi.org/10.30756/ahmj.2020.01.02
Received Date: Dec 2, 2019
Accepted Date: Dec 6, 2019
Published Date: Dec 13, 2019
Recommended Citation: Chen PM, Ben-Haim S, Handwerker J, Ansari H.Cluster-Tic or Tic-Cluster? Trigeminal Neuralgia (Tic) Turning to Trigeminal Autonomic Cephalalgia (TAC) Following Venous Decompression of the Trigeminal Nerve: A Case Report and Review of the Literature. Ann Head Med. 2020;01:02. DOI: 10.30756/ahmj.2020.01.02
Objective: We present a rare case of Tic-cluster in the context of venous compression of the trigeminal nerve.
Background: Cluster-Tic syndrome is a rare headache condition with features of both trigeminal neuralgia (Tic) and trigeminal autonomic cephalalgia symptom (TAC).
Methods: Case report and review of literature.
Results: A 75-year old man presents with left sided paroxysmal pain consistent with trigeminal neuralgia (Tic). Magnetic resonance demonstrated a venous compression of the posterior-medial aspect of the left trigeminal ganglion. He underwent microvascular decompression which confirmed petrosal vein compression with subsequent symptomatic resolution. After two years of remission, he had a new left unilateral throbbing headache consistent with International Classification of Headache Disorders (ICHD)- 3 cluster headache definition, which improved with steroids.
Conclusion: Cluster-Tic syndrome has variable clinical presentations. Tic can precede cluster and the possible role of venous trigeminal compression in this headache remains unclear.
Introduction
“Cluster-Tic” syndrome is a term used to describe the rare spectrum overlap of pain attacks resembling trigeminal neuralgia (Tic) and cluster or other trigeminal autonomic cephalalgia type pain (TAC)1 2. These can precede one another or co-exist. We present an unusual case of Tic-cluster syndrome with Tic symptoms that went into complete remission following trigeminal nerve decompression then independent occurrence of new cluster symptomatology.
Case
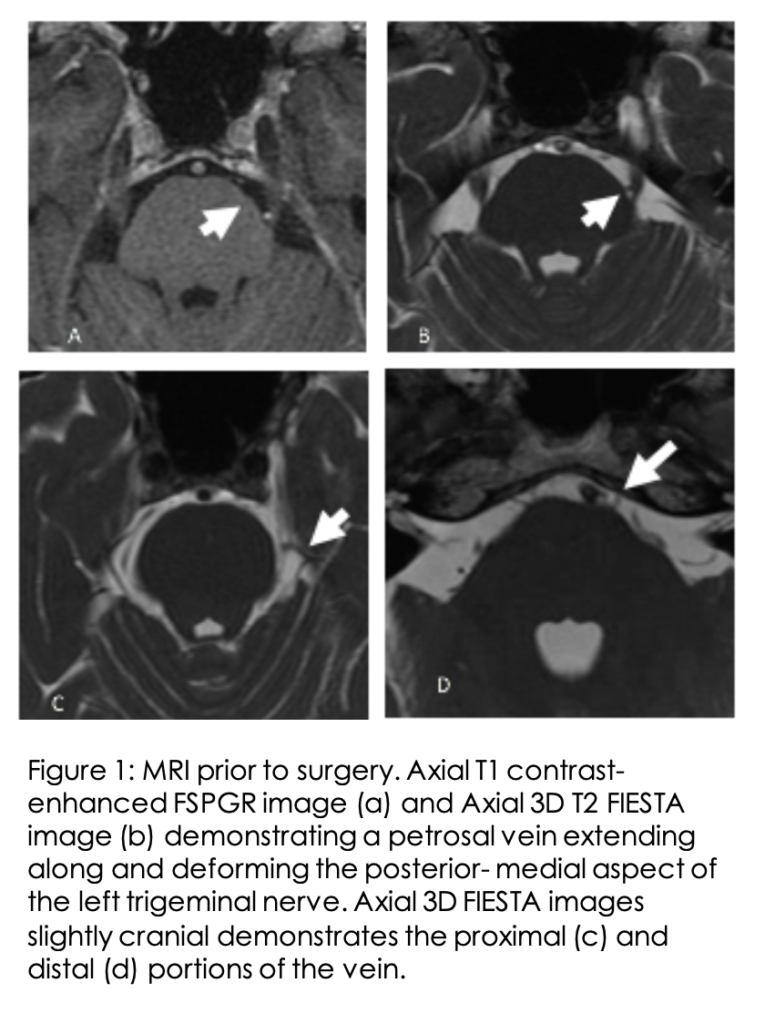
A 75-year old man initially presented to his primary care provider with left sided facial pain. The pain was described as throbbing, stabbing and piercing and involved the left V2-V3 distributions with some radiation to V1. This pain lasts less than 2 minutes, occurs multiple times a day, and is provoked by teeth brushing and shaving. His initial neurologic exam was otherwise unremarkable. He was treated with carbamazepine for trigeminal neuralgia with minimal improvement. The dose of carbamazepine could not be increased to more than 400 mg per day due to significant side effects. He was then treated with local glycerolysis with transient improvements. MRI brain demonstrated no abnormal mass lesions or enhancement along the trigeminal nerves, though there was thought to be possible vascular compression of the left trigeminal ganglion by petrosal vein [Figure 1].
He subsequently underwent left retromastoid craniectomy with microvascular decompression of the left trigeminal nerve. Of note, intra-operatively there was a petrous vein extending from the junction of the tentorium and petrous bone sweeping under the trigeminal nerve. The nerve appeared to be distorted upwards by the superior petrosal vein. The vein was therefore dissected from the surrounding adhesions, coagulated and cut. Subsequently the nerve appeared to be decompressed, and there were no additional vascular structures noted near the root entry zone.
He had near complete resolution of trigeminal pain (Tic) symptoms following the microvascular decompression surgery. Two years following surgery he developed a throbbing left retro-orbital pain localized to the V1 distribution. There was associated left conjunctival redness and agitation with observed mydriasis per family members during the headache attacks. He had 1 to 8 attacks per day ranging from 15 to 90-minute duration and triggered by sleep. There was no sharp, shooting or jabbing pain. There were no cutaneous stimulation triggers and no teeth brushing or chewing triggers. A nine-day trial of indomethacin (dose up to 200 mg per day) to rule out paroxysmal hemicrania was initiated without improvement. He was subsequently started on 60 mg of oral prednisone for suspected cluster headache with complete remission of symptoms. Therefore, prednisone was tapered and stopped after a 3 weeks course.
The patient remained pain-free at the 3- and 6-months follow up visits. The patient has consented to publication of this case.
Discussion
We present a patient with initial trigeminal neuralgia (Tic) that went into remission following petrosal vein decompression at trigeminal entry zone, with subsequent delayed cluster headache development.
The ICHD-3 places cluster-tic syndrome as a comment under cluster headache and trigeminal neuralgia, noting that the patient should receive both diagnoses and be treated respectively for each etiology 1. There are approximately 50 cases reported 3. Aspects of this case that are unique include the initial Tic transformed to cluster headache.
This patient initially fit the following ICHD-3 criteria for trigeminal neuralgia: innocuous stimuli and short paroxysmal shooting pains with episodes of remission. This was not consistent with Short-lasting unilateral neuralgiform headache with conjunctival injection and tearing (SUNCT) mainly because of the V2-V3 distribution, lack of autonomic feature and presence of cutaneous trigger. The clinical differentiation of Tic and SUNCT is difficult and a previous meta-analysis notes the grouping of Tic and SUNCT as one syndrome 4. It is possible there is an underestimation of SUNCT-Tic and overrepresentation of cluster-Tic. This is further supported by the high preponderance in the literature of isolated V1 segment involvement which was not seen in this patient.
The second headache appears to be most consistent with cluster headache subtype of TAC using the ICHD-3 definition 1. In particular, this patient had at least 5 attacks and each attack last about 15 minutes. The attacks frequency is up to 8 attacks per day with nocturnal timing and associated unilateral autonomic features (conjunctival congestion and pupillary change). It seems unlikely that the cluster headache is independent of the onset of initial tic. A primary cluster headache in this age demographic is remarkably unlikely 5 . The proximity to a trigeminal surgery suggests the possibility of a secondary cluster. Nevertheless, cluster headache is thought to originate from the posterior hypothalamus 6. Post-surgical cluster has been reported after carotid endarterectomy 7, though trigeminal surgical decompression does not involve the hypothalamic or sympathetic chain regions.
The majority of cluster-tic cases have concomitant tic and TAC syndrome. A delayed transition of independently occurring Tic to TAC, as in this case, is rare. A cross sectional study demonstrated only 1.2% of patients with trigeminal neuralgia and cluster headache episodes occurring independently 8. This patient had trigeminal neuralgia pain for 1 year in isolation, with a 2-year delay before the development of cluster symptoms. A meta-analysis showed the range of delay was 8 months to 3 year 9 2 10.
The age of onset in this case is a distinguishing factor. There is a wide age range of cluster-tic, occurring from age 20 to 79. Our patient is the oldest to have a time dispersion between Tic and TAC. Only one other case was a 35-year-old woman with temporal delay between the trigeminal neuralgia (affecting V1, V2, V3 divisions) and subsequent cluster headache 11 . Also, the fact that in our case TAC (Cluster) developed after trigeminal neuralgia (Tic) made this case unique.
An interesting point is the drastic improvement in trigeminal neuralgia symptoms after surgical decompression. Venous compression trigeminal neuralgia is relatively rare and controversial, occurring in isolation in 8.3% during microvascular decompressions 12. Only one previous case report has implicated venous compression in cluster-tic. In that case the authors described a patient who had first trigeminal, then SUNCT then finally cluster symptoms 13 . This ‘Tic- SUNCT-Cluster” syndrome went into remission after petrosal vein decompression. In the limited 3 cases of trigeminal surgery for cluster tic syndrome there was in general non sustained improvement 11 14. The decompressed patients in the other cases demonstrated both trigeminal neuralgia and TAC symptoms simultaneously. This case adds to the heterogenicity of response to decompression in cluster-TIC and a number of questions remain including: if cluster tic shares pathophysiologic similarities to each independent pathology, if remission with delayed cluster is coincidental or if decompression plays a role in kindling a cluster subtype. It is possible that there is a compressive subtype of Tic-Cluster. This case points to a need to further investigate this potential relationship.
The underlying shared pathophysiology of Tic and TACs is unknown and controversial. A proposed possibility is that an abnormal hypothalamic relay may lead to activation of the trigeminal nucleus caudalis 6. While it is possible that a cluster-tic patient may in fact have each condition individually due to shared comorbidity, each condition is respectively rare. The possibility of an underlying unknown linking etiology (e.g. genetics or environmental) is further supported by the shared trigeminal localization and cases of Tic to SUNCT transition. A solely peripheral mechanism has been extensively debated 15 . This case seems to support a shared pathology involving the trigeminal nerve between Tic and TAC given the unique involvement of decompressive surgery in our case.
In summary, we have demonstrated a likely diagnosis of tic-cluster syndrome despite a delay of years between symptoms. This case highlights the nuances in the diagnosis of tic-cluster and the challenging variability in the tic-cluster clinical phenotype.
References
- The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013; 33: 629-808. 2013/06/19. DOI: 10.1177/0333102413485658. PubMed CrossRef GoogleScholar
- Klimek A. Cluster-tic syndrome. Cephalalgia 1987; 7: 161-162. 1987/06/01. DOI: 10.1046/j.1468-2982.1987.0702161.x. PubMed CrossRef GoogleScholar
- Wober C. Tics in TACs: A Step into an Avalanche? Systematic Literature Review and Conclusions. Headache 2017; 57: 1635-1647. 2017/05/26. DOI: 10.1111/head.13099. PubMed CrossRef GoogleScholar
- VanderPluym J and Richer L. Tic versus TAC: differentiating the neuralgias (trigeminal neuralgia) from the cephalalgias (SUNCT and SUNA). Curr Pain Headache Rep 2015; 19: 473. 2014/12/17. DOI: 10.1007/s11916-014-0473-9. PubMed CrossRef GoogleScholar
- Rozen TD and Fishman RS. Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache 2012; 52: 99-113. 2011/11/15. DOI: 10.1111/j.1526-4610.2011.02028.x. PubMed CrossRef GoogleScholar
- Leone M, Mea E, Genco S, et al. Coexistence of TACS and trigeminal neuralgia: pathophysiological conjectures. Headache 2006; 46: 1565-1570. 2006/11/23. DOI: 10.1111/j.1526-4610.2006.00537.x. PubMed CrossRef GoogleScholar
- Dirkx TH and Koehler PJ. Post-Operative Cluster Headache Following Carotid Endarterectomy. Eur Neurol 2017; 77: 175-179. 2017/02/06. DOI: 10.1159/000456004. PubMed CrossRef GoogleScholar
- Wilbrink LA, Weller CM, Cheung C, et al. Cluster-tic syndrome: a cross-sectional study of cluster headache patients. Headache 2013; 53: 1334-1340. 2013/07/03. DOI: 10.1111/head.12161. PubMed CrossRef GoogleScholar
- Watson P and Evans R. Cluster-tic syndrome. Headache 1985; 25: 123-126. 1985/05/01. DOI: 1111/j.1526-4610.1985.hed2503123.x . PubMed CrossRef GoogleScholar
- Monzillo PH, Sanvito WL and Da Costa AR. Cluster-tic syndrome: report of five new cases. Arq Neuropsiquiatr 2000; 58: 518-521. 2000/08/02. DOI: 10.1590/s0004-282×2000000300019 . PubMed CrossRef GoogleScholar
- Solomon S, Apfelbaum RI and Guglielmo KM. The cluster-tic syndrome and its surgical therapy. Cephalalgia 1985; 5: 83-89. 1985/06/01. DOI: 10.1046/j.1468-2982.1985.0502083.x. PubMed CrossRef GoogleScholar
- Dumot C, Brinzeu A, Berthiller J, et al. Trigeminal neuralgia due to venous neurovascular conflicts: outcome after microvascular decompression in a series of 55 consecutive patients. Acta Neurochir (Wien) 2017; 159: 237-249. 2016/11/07. DOI: 10.1007/s00701-016-2994-y. PubMed CrossRef GoogleScholar
- de Coo I, van Dijk JM, Metzemaekers JD, et al. A Case Report About Cluster-Tic Syndrome Due to Venous Compression of the Trigeminal Nerve. Headache 2017; 57: 654-657. 2016/12/08. DOI: 10.1111/head.12990. PubMed CrossRef GoogleScholar
- Alberca R and Ochoa JJ. Cluster tic syndrome. Neurology 1994; 44: 996-999. 1994/06/01. PubMed CrossRef GoogleScholar
- Goadsby PJ and Lipton RB. Paroxysmal hemicrania-tic syndrome. Headache. United States, 2001, pp.608-609. PubMed CrossRef GoogleScholar
Disclosures
Consent was obtained by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
