Author: Mohammed Wulgo Ali, MBBS * MBBS 1, Umar Baba Musami MBBS, MSc 2,3, Fatima Abba Ali MBBS 3, Sahabi Kabir Sulaiman MBBS 4
Author Affiliation:
1 College of Medical Sciences, Gombe State University, Nigeria
2 College of Medical Sciences, University of Maiduguri, Nigeria
3 Federal Neuropsychiatric Hospital Maiduguri, Nigeria
4 Yobe State University Teaching Hospital Damaturu, Nigeria
Competing Interests: The author/s declare no competing interests.
Issue: 07.02
DOI: 10.30756/ahmj.2022.07.02
Received: Apr 22, 2022
Revised: May 13, 2022
Accepted: May 17, 2022
Published: May 27, 2022
Recommended Citation: Ali MW, Musami UB, Ali FA, Sulaiman SK. Comorbid Depression Among Patients with Migraine in Low Resource Setting. Ann Head Med. 2022;07:02. DOI: 10.30756/ahmj.2022.07.02
Background and objectives: Migraine is commonly associated with psychiatric comorbidities, especially in developed countries. Herein, we investigated the burden of comorbid depression and associated factors among patients with migraine (PWM) in low resource setting.
Methods: This was a hospital-based cross-sectional study of PWM conducted at Federal Neuropsychiatric Hospital (FNPH) Maiduguri. Consenting participants with known migraine on follow up visits were consecutively recruited. Depressive symptoms were ascertained using the Beck’s Depression Inventory (BDI), while the impact of migraine was assessed using the Headache Impact Test-6 (HIT-6) questionnaire. Multivariate regression analysis was done to determine independent factors associated with depression among migraineurs.
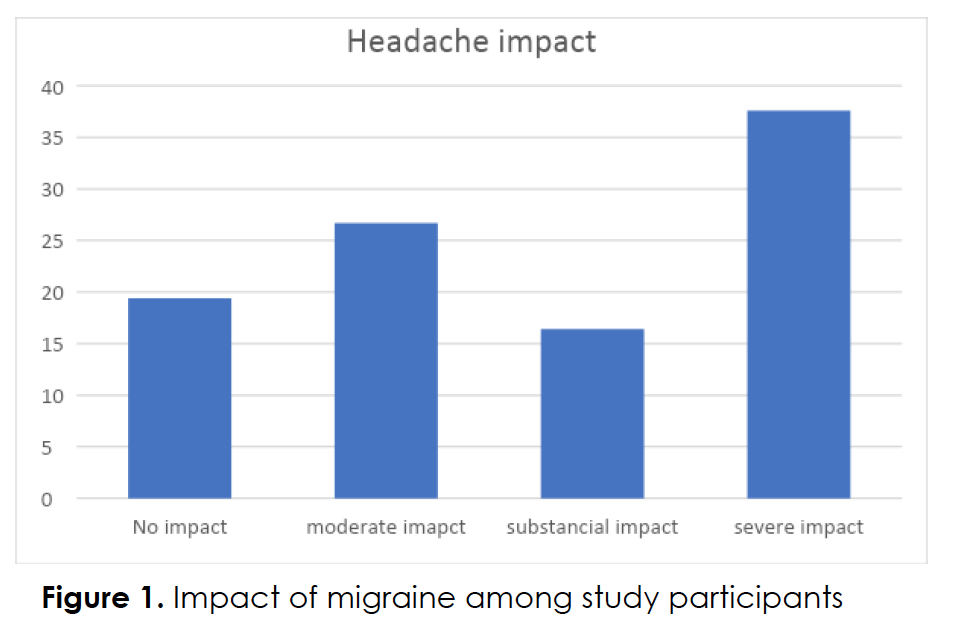
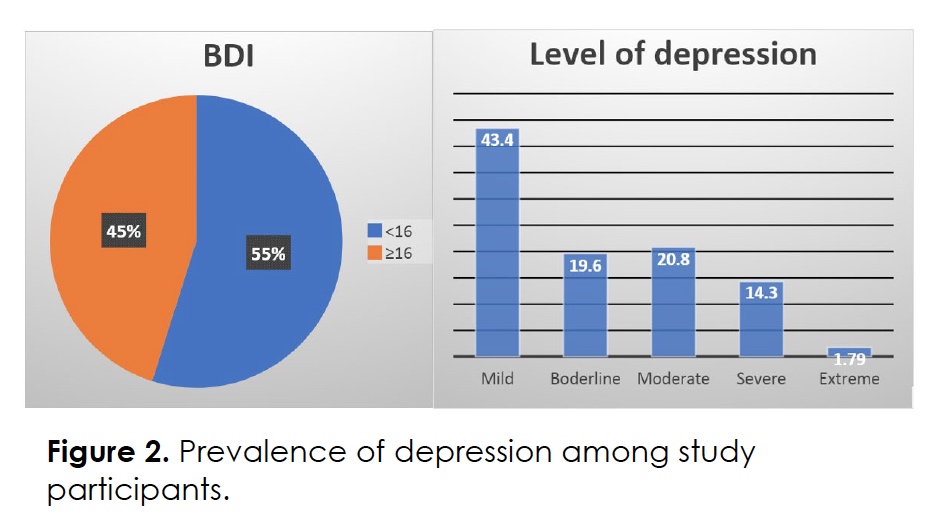
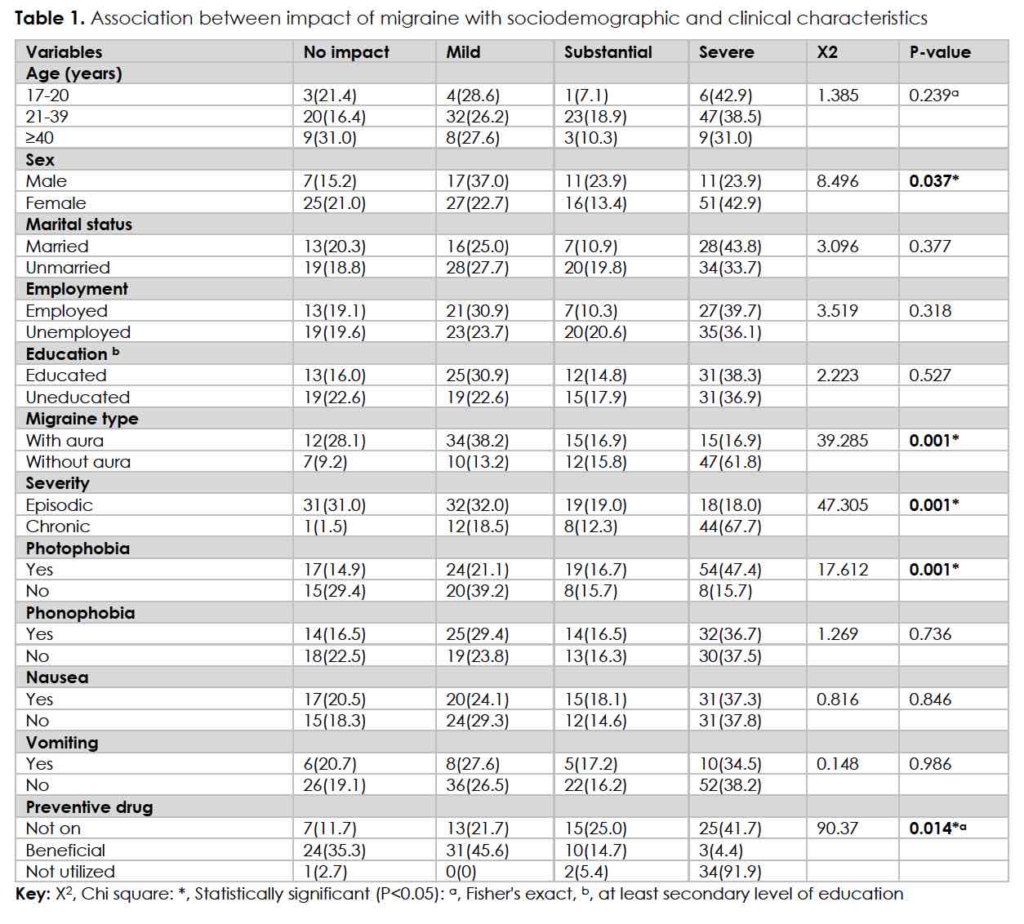
Results: The study constituted 165 PWM. Participants were predominantly females (72.1%) and the mean age of the participants was 29.6 ± 9.6, with age range of 17-55 years. About 46% of migraineurs had mild to no impact, while 37.6% of the participants had severe headache impact. Increased migraine impact was associated with: female gender (P<0.037), migraine with aura (P<0.001), chronic migraine (P<0.001), photophobia (P<0.001), and poor utilization of prophylactic drugs (P<0.014). Forty-five percent of the participants had varying degrees of depression among which the majority (43.4%) had mild, 19.6% moderate, 14.3% severe, and 1.79% had extreme comorbid depression. Factors associated with depression were: female gender, migraine with aura, chronic migraine, photophobia, utilization of migraine prophylactic drugs, and impactful migraine all with P≤0.001. We found a strong positive linear relationship between headache impact and depression (r=0.76, P<0.001). On multivariate analysis, males had 76.3% less likelihood of being depressed [95% confidence interval (CI) of (0.068-0.828)] compared with their female counterparts. Increasing migraine impact was also significantly (P<0.05) associated with depression. Those with no impact, mild impact, and substantial impact of migraine had 97.4%, 97.1%, and 88.4% less likelihood of being depressed compared to those with severe impact with 95% CI (0.004-0.159), (0.006-0.148)], and (0.029-0.463)] respectively.
Conclusion: We found a high prevalence of comorbid depression among PWM in our environment with inadequate utilization of treatment contributing to both the burden of migraine and depression.
Introduction
Migraine is a common neurologic disorder with an estimated prevalence of more than a billion population globally 1. In 2015, nearly half to two-thirds of adults aged 18-65 years globally have had headache, with migraine reported to account for over 3 in every 10 of such headaches 2. The difference in methodology and population studied has yielded a varied migraine prevalence range of 13.1-45.8% in sub-Saharan Africa 3-8. Migraine is the 7th disabling disease and the most common cause of disability in individuals aged 15-49 years 9, 10 A disability adjusted life years (DALYs) as high as 16.3% has been reported for migraine, making it the second largest contributor of neurological DALYs after stroke (42.2%) 11. The optimal care of migraine sufferers in sub-Saharan Africa is largely hindered by unawareness of the condition, significant avoidable delay before migraine diagnosis, unavailability of medication, or presentation with migraine complication 12.
Migraine symptoms often interfere with socioeconomic functions and are associated with psychiatric comorbidities such as depression and anxiety 13, 14. Like migraine, depression is also a serious disabling disorder with an umpteen socioeconomic burden. Depression affects nearly 3 in every 10 people, and between 76% to 85% of people with depression in low- and middle-income (LMIC) received no treatment for their disorder 15. Studies have shown a reciprocal complex relationship between migraine and depression with a potential of each disorder triggering the other 16, 17. The symptoms of sleep and appetite disturbance, weight changes, sadness, lack of concentration and motivation associated with depression can serve as migraine trigger/ symptoms hence further contributing to chronification of migraine and can negatively affect quality of life (QoL). Population-based studies had reported that people suffering from both migraine and depression had poorer health-related outcomes and respond less effectively to migraine treatment compared with those without comorbid psychiatric disorders 18-20. Identified risk factors for depression among migraineurs include female sex, photophobia, chronic migraine, and difficult to treat migraine 21. There is paucity of studies evaluating the impact of comorbid depression among patients with migraine (PWM) in sub-Saharan Africa. Hence, this has piqued interest to determine the prevalence of depression among migraineurs and further evaluate other associated factors with the aim of identifying burden of depression among PWM and recommend measures for individualized and holistic treatment of sufferers to improve their quality of care.
Methods
Study Setting And Participants
This was a hospital-based cross-sectional study conducted between January, 2021 to August, 2021 at Federal Neuropsychiatric Hospital (FNPH) Maiduguri, North East Nigeria. Approval for the study was obtained from the ethics and research committee of the institution prior to commencement of the study. Participants with known migraine were recruited consecutively from the outpatient clinic at the time of their follow up visits and the purpose of the study explained in clear terms. Consenting subjects had their demographic variables consisting of age, sex, marital status, educational status (participants that had completed at least secondary level education were considered educated), and occupation captured on a structured questionnaire. Participants were further interviewed with the Becks Depression Inventory (BDI) questionnaire and the impact of migraine was assessed using Headache Impact Test 6 (HIT-6). Excluded from the study were those known to have psychiatric illness or cognitive impairment, pregnant and lactating mothers, and participants known to have other systemic comorbidities.
Study Instruments
HIT-6: This is a widely used and validated patient reported outcome measure (PROM) that quantifies the impact of headache on the quality of life of the individual under several conditions of daily living that includes activities at home, work, studies, and social situations. The score obtained indicates the level of impact of headaches: 36 to 49 points suggests little-to-no impact, 50 to 55 points moderate impact while 56 to 59 suggests substantial impact, and values greater than 60 points indicates severe impact.
Beck’s Depression Inventory (BDI): This is a commonly used self-rating scale for depression. Participants rated 21 items on a scale from 0 to 3 according to how they felt at the time. Subjects who scored above 16 were considered to have depression. The BDI has been standardized and widely adopted in Nigeria 22-24.
Data analysis: data was analyzed using IBM SPSS (Chicago, Illinois) software version 23. Frequency tables were generated for the categorical variables. For descriptive statistical methods, proportions with 95% confidence intervals were used. The mean was used to determine the measure of central tendency of the continuous variables. Intergroup differences in data were tested for significance using chi-square test for proportions. Multivariable logistic regression model was used to determine dependent variables. A P value of <0.05 was considered statistically significant.
Results
During the study period, 165 participants who fulfilled the ICD 3 criteria for migraine headache were recruited. The participants consisted of 119 (72.1%) females, and 46 (27.9%) males with a female to male ratio of 2.6:1. The mean age of the participants was 29.6 ± 9.6 with an age range of 17-55 years, and 73.9% were within the age range of 20-40 years. Most (61.2%) of the participants were unmarried, and 58.8% are without income. About half of the study participants were educated. A majority (60.6%) of the participant had fulfilled the criteria for episodic migraine. The mean HIT-6 score was 56.8 ± 7.59, and most of the participants had severe headache impact (37.6%), while 16.4 % had substantial impact, 27.3 % had moderate impact, and 18.8 % had no migraine impact as shown in Figure 1. Significant statistical association was found between increased migraine impact with female gender (P=0.037), type of migraine (P≤0.001), duration of migraine (P≤0.001), photophobia (P≤0.001), and utilization of migraine prophylactic medication (P=0.014) as shown in Table 1.
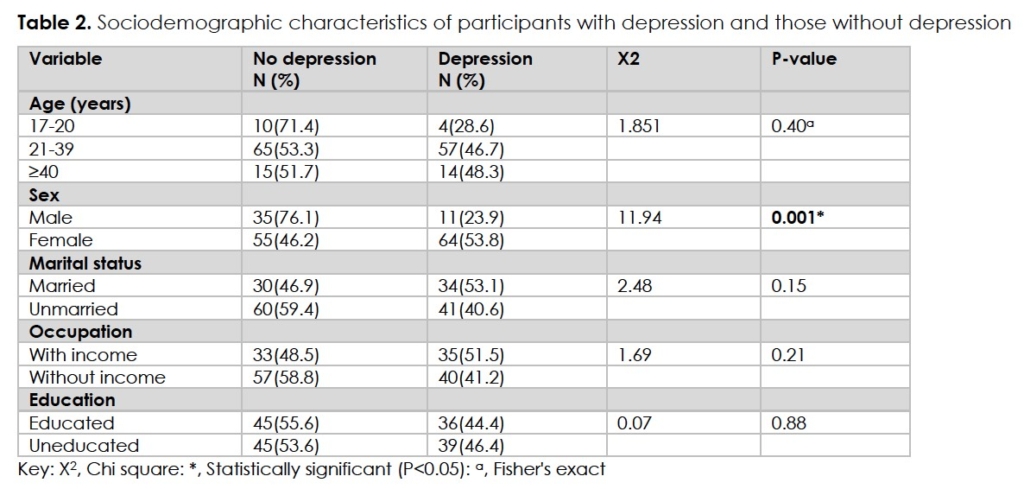
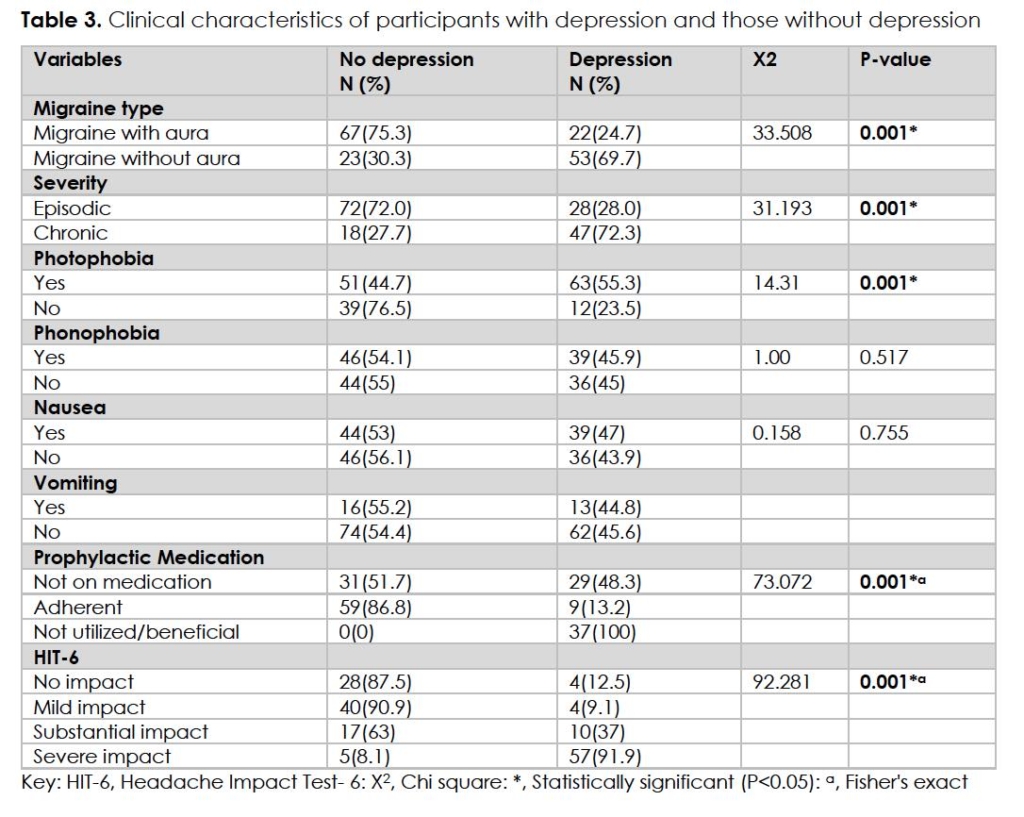
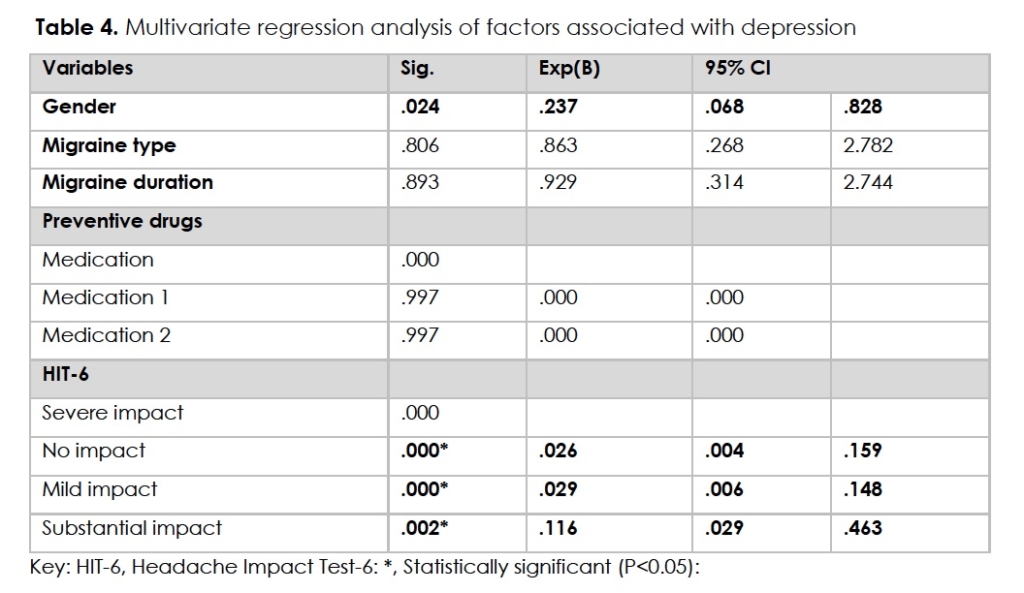
About 45% of the participants were identified to have various degrees of comorbid depression among which the majority (43.4%) had mild depression, 19.6% borderline depression, 20.8% moderate depression, 14.3% severe depression, and 1.79% had extreme depression (Figure 2). Factors associated with depression (Tables 2,3) were; migraine without aura (P≤0.001), chronic migraine (P≤0.001), photophobia (P≤0.001), poor utilization of prophylactic drugs (P≤0.001), and impactful migraine (P≤0.001). We found a strong positive linear relationship between headache impact and depression (r=0.76, P<0.001). On multivariate analysis (Table 4), males had 76.3% less likelihood of being depressed [95% confidence interval (CI) of (0.068-0.828)] compared with female gender. Increasing migraine impact was also significantly (P<0.05) associated with depression. Those with no impact, mild impact, and substantial impact of migraine had 97.4%, 97.1%, and 88.4% less likelihood of being depressed compared to those with severe impact with 95% CI (0.004-0.159), (0.006-0.148)], and (0.029-0.463)] respectively.
Tables
Discussion
The present study assessed the prevalence of depression among PWM and the effects of sociodemographic and clinical factors, and impact of migraine on comorbid depression in Northeast Nigeria. According to the findings of this study, 46.1% of migraineurs had mild to no impact, while 37.6% of the participants had severe headache impact. Forty-five percent of the participants had varying degrees of comorbid depression that was significantly associated with gender, migraine type, duration of migraine history, photophobia, utilization of migraine preventive medications, and increasing impact of migraine. On further multivariate logistic regression analysis, female gender and worsening impact of migraine was found to be independently associated with depression among PWM.
The mean age of our study participants is comparable to other studies among migraineurs in Nigeria and beyond, signifying more affectation of younger individuals 12, 16. The observed female predominance in this study is in keeping with earlier published studies supporting affectation of more females compared with their male counterparts 4-6. Studies have also established a disproportionately higher occurrence of headache-related disabilities among females. The gender disparity in prevalence and headache-related disabilities among females has been attributed to modulatory effects of sex hormones on migraine susceptibility 25, 26.
In comparison with other studies, the prevalence of comorbid depression among migraineurs in our study is higher than previous reports of 27.74% by Sevillano-García et al and 36% by Krashin et al respectively 27, 28. Cardona-Castrillon et al reported a significantly lower prevalence of 21.3% for major depressive among migraineurs with 4.5% of their participants having dysthymic disorders 29. The variations in prevalence of comorbid depression might largely result from methodologic difference among recruited participants in relation to sample size, sociodemographic/ socioeconomic differences, and application of the study tools in assessing depression. However, the high proportion of patients with chronic migraine and significant headache impact in this our clinic-based study can contribute to the high prevalence of depression that was found.
Our finding of the association between migraine without aura and depression was similarly reported by Sevillano-Garcia et al 27. Contrary to these findings is the reports of Radar and colleagues 30, they further reported a more significant association of migraine with aura with major depressive and anxiety disorders. Llop et al similarly found that patients with interictal photophobia are more likely to be depressed than those without interictal photophobia 21. The results of our study have shown depression among PWM is closely associated with CM. This finding agrees with that of Buse et al, where they found psychiatric disorders among PWM were more prevalent in those with CM than EM in both clinic- and population-based studies 28. On further regression analysis, we reported that female were three times more likely to be depressed compared to their male counterpart. In a study conducted to determine comorbidity of migraine with four psychiatric conditions (depression, anxiety, stress and insomnia), they discovered that the odds for depression and anxiety were higher among women, while stress and anxiety was the same for both sexes 27. The results from our study further revealed that increasing impact of migraine as measured by the HIT-6 was strongly associated with co-morbid depression in the studied population. This was evident by the fact that those with no impact, mild impact and substantial impact had less likelihood of being depressed when compared to those with severe impact. In a study by Buse et al, people with CM (specifically) had a significantly greater likelihood of experiencing severe headache impact and also had more chances of higher adverse headache impact, with depression as one of the predictors of headache impact adversity that is common for both CM and EM 31. On the other hand, Tomé-Pires et al. reported no association between migraine headache impact and depression but found association between migraine and anxiety 32.
Limitations of the study are the sampling technique and cross-sectional design which cannot validate causality of the associations between the outcome variable and independent variables. Migraineurs with moderate to severe headache are more likely to be seen in specialist clinics, and it is also likely that recruited participants on follow up had recent attacks of headache which can also interfere with their responses. The results of this clinic-based study, with its limited sample size cannot be generalized to the population of all PWM in low resource settings. However, this study has provided important insights on the burden of depression among migraineurs in sub-Saharan Africa.
Conclusion
The findings from this study further emphasizes the occurrence of high prevalence of comorbid depression among people living with migraine in our environment with inadequate utilization of treatment contributing to both the burden of migraine and depression. This buttresses the need for instituting routine screening of depressive symptoms as part of care and a need for multidisciplinary approach of treatment.
Acknowledgement
We acknowledge with gratitude the patience of our study participants despite their adversaries of living with migraine especially in our resource limited setting. The authors also acknowledge the contributions of the nurses and medical record staff of FNPH Maiduguri. We also appreciate the intellectual contributions of Marco Lisicki while preparing the manuscript.
Declarations/Disclosures
Ethical Approval: Approval for the study was obtained from the Health Research and Ethics Committee (approval no: FNPH/032020/REC042), Federal Neuropsychiatric Hospital Maiduguri, Nigeria. The research was performed in accordance with the Declaration of Helsinki.
Consent/Permissions: All participants gave informed consent before taking part in the study.
Funding: None.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, author declares the following:
Payment/services info: Author has declared that no financial support was received from any organization for the submitted work.
Financial relationships: Author have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: Author have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
- Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. Sep 16 2017;390(10100):1211-1259. PubMed PMID: 28919117; PubMed Central PMCID: PMCPMC5605509. doi:10.1016/S0140-6736(17)32154-2
- Headache disorders. WHO Fact Sheet Accessed May 20, 2022. https://www.who.int/news-room/fact-sheets/detail/headache-disorders
- Onwuekwe I, Onyeka T, Aguwa E, Ezeala-Adikaibe B, Ekenze O, Onuora E. Headache prevalence and its characterization amongst hospital workers in Enugu, South East Nigeria. Head Face Med. Nov 25 2014;10:48. PubMed PMID: 25423879; PubMed Central PMCID: PMCPMC4289241. doi:10.1186/1746-160X-10-48
- Ojini FI, Okubadejo NU, Danesi MA. Prevalence and clinical characteristics of headache in medical students of the University of Lagos, Nigeria. Cephalalgia. Apr 2009;29(4):472-7. PubMed PMID: 19170698. doi:10.1111/j.1468-2982.2008.01766.x
- Zebenigus M, Tekle-Haimanot R, Worku DK, Thomas H, Steiner TJ. The prevalence of primary headache disorders in Ethiopia. J Headache Pain. Dec 2016;17(1):110. PubMed PMID: 27924616; PubMed Central PMCID: PMCPMC5142157. doi:10.1186/s10194-016-0704-z
- Oshinaike O, Ojo O, Okubadejo N, Ojelabi O, Dada A. Primary headache disorders at a tertiary health facility in Lagos, Nigeria: prevalence and consultation patterns. Biomed Res Int. 2014;2014:782915. PubMed PMID: 24587991; PubMed Central PMCID: PMCPMC3920920. doi:10.1155/2014/782915
- Mbewe E, Zairemthiama P, Yeh HH, Paul R, Birbeck GL, Steiner TJ. The epidemiology of primary headache disorders in Zambia: a population-based door-to-door survey. J Headache Pain. 2015;16:515. PubMed PMID: 25916334; PubMed Central PMCID: PMCPMC4401479. doi:10.1186/s10194-015-0515-7
- Omogbiya AI AK, Umukoro EK, Moke EG, Nzei A. . Academic-related stress and prevalence of migraine and tension-type headaches amongst undergraduates of Delta State University, Abraka, Nigeria. Res J of Health Sci. 2020;8(2):133-145. doi:10.4314/rejhs.v8i2.9
- Steiner TJ, Stovner LJ, Birbeck GL. Migraine: the seventh disabler. Headache. Feb 2013;53(2):227-9. PubMed PMID: 23317094. doi:10.1111/head.12034
- Steiner TJ, Stovner LJ, Vos T, Jensen R, Katsarava Z. Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain. Feb 21 2018;19(1):17. PubMed PMID: 29468450; PubMed Central PMCID: PMCPMC5821623. doi:10.1186/s10194-018-0846-2
- Intersectoral Global Action Plan on epilepsy and other neurological disorders 2022 – 2031. WHO. Accessed May 24, 2022. https://www.who.int/publications/m/item/intersectoral-global-action-plan-on-eepilepsy-and-other-neurological-disorders-2022-2031
- Ali MW, Musami, U.B., Sa’ad, F.K. et al. Profile of Migraine Patients in a Developing Country: a Multicentre Study. SN Compr Clin Med. 2020;2:1153–1157. doi:10.1007/s42399-020-00394-x
- McLean G, Mercer SW. Chronic migraine, comorbidity, and socioeconomic deprivation: cross-sectional analysis of a large nationally representative primary care database. J Comorb. 2017;7(1):89-95. PubMed PMID: 29299439; PubMed Central PMCID: PMCPMC5695976. doi:10.15256/joc.2017.7.114
- Minen MT, Begasse De Dhaem O, Kroon Van Diest A, et al. Migraine and its psychiatric comorbidities. J Neurol Neurosurg Psychiatry. Jul 2016;87(7):741-9. PubMed PMID: 26733600. doi:10.1136/jnnp-2015-312233
- WHO Fact Sheet on Depression. WHO. Accessed May 24, 2022. https://www.who.int/news-room/fact-sheets/detail/depression
- Domingues RB, Costa EA, Silva A, Jr., et al. Correlation between migraine subtypes and depression. Arq Neuropsiquiatr. Sep 2008;66(3A):485-7. PubMed PMID: 18813705. doi:10.1590/s0004-282×2008000400009
- Hamelsky SW, Lipton RB. Psychiatric comorbidity of migraine. Headache. Oct 2006;46(9):1327-33. PubMed PMID: 17040330. doi:10.1111/j.1526-4610.2006.00576.x
- Jette N, Patten S, Williams J, Becker W, Wiebe S. Comorbidity of migraine and psychiatric disorders–a national population-based study. Headache. Apr 2008;48(4):501-16. PubMed PMID: 18070059. doi:10.1111/j.1526-4610.2007.00993.x
- Breslau N, Davis GC. Migraine, physical health and psychiatric disorder: a prospective epidemiologic study in young adults. J Psychiatr Res. Apr-Jun 1993;27(2):211-21. PubMed PMID: 8366470. doi:10.1016/0022-3956(93)90009-q
- Lanteri-Minet M, Radat F, Chautard MH, Lucas C. Anxiety and depression associated with migraine: influence on migraine subjects’ disability and quality of life, and acute migraine management. Pain. Dec 5 2005;118(3):319-326. PubMed PMID: 16289799. doi:10.1016/j.pain.2005.09.010
- Llop SM, Frandsen JE, Digre KB, et al. Increased prevalence of depression and anxiety in patients with migraine and interictal photophobia. J Headache Pain. 2016;17:34. PubMed PMID: 27080113; PubMed Central PMCID: PMCPMC4831954. doi:10.1186/s10194-016-0629-6
- A A. The Beck depression Inventory in relation to some commonly used tests in Nigeria. Nigerian J Basic Appl Psychol. 1988;1:23-28.
- Ibrahim AW WM, Jidda MS, Omeiza BA, Pindar SK, Rabbebe IB, Yusuph H. Predictors of Depression And Psychometric Evaluation of the Beck Depression Inventory-II (BDI-II) Among Adults on Highly Active Antiretroviral Therapy In Maiduguri, North-Eastern Nigeria. Bo Med J. 2014;11(1):1-16.
- Adewuya AO, Ola BA, Aloba OO. Prevalence of major depressive disorders and a validation of the Beck Depression Inventory among Nigerian adolescents. Eur Child Adolesc Psychiatry. Aug 2007;16(5):287-92. PubMed PMID: 17473949. doi:10.1007/s00787-006-0557-0
- Victor TW, Hu X, Campbell JC, Buse DC, Lipton RB. Migraine prevalence by age and sex in the United States: a life-span study. Cephalalgia. Sep 2010;30(9):1065-72. PubMed PMID: 20713557. doi:10.1177/0333102409355601
- Buse DC, Loder EW, Gorman JA, et al. Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache. Sep 2013;53(8):1278-99. PubMed PMID: 23808666. doi:10.1111/head.12150
- Sevillano-Garcia MD, Manso-Calderon R, Cacabelos-Perez P. [Comorbidity in the migraine: depression, anxiety, stress and insomnia]. Rev Neurol. Oct 1-15 2007;45(7):400-5. Comorbilidad en la migrana: depresion, ansiedad, estres y trastornos del sueno. PubMed PMID: 17918105.
- Buse DC, Silberstein SD, Manack AN, Papapetropoulos S, Lipton RB. Psychiatric comorbidities of episodic and chronic migraine. J Neurol. Aug 2013;260(8):1960-9. PubMed PMID: 23132299. doi:10.1007/s00415-012-6725-x
- Cardona-Castrillon GP, Isaza R, Zapata-Soto AP, Franco JG, Gonzalez-Berrio C, Tamayo-Diaz CP. [The comorbidity of major depressive disorder, dysthymic disorder and anxiety disorders with migraine]. Rev Neurol. Sep 1-15 2007;45(5):272-5. Comorbilidad de trastorno depresivo mayor, trastorno distimico y trastornos de ansiedad con migrana. PubMed PMID: 17876737.
- Radat F, Swendsen J. Psychiatric comorbidity in migraine: a review. Cephalalgia. Mar 2005;25(3):165-78. PubMed PMID: 15689191. doi:10.1111/j.1468-2982.2004.00839.x
- Buse D, Manack A, Serrano D, et al. Headache impact of chronic and episodic migraine: results from the American Migraine Prevalence and Prevention study. Headache. Jan 2012;52(1):3-17. PubMed PMID: 22106869. doi:10.1111/j.1526-4610.2011.02046.x
- Tome-Pires C, Sole E, Racine M, et al. The relative importance of anxiety and depression in pain impact in individuals with migraine headaches. Scand J Pain. Oct 2016;13:109-113. PubMed PMID: 28850506. doi:10.1016/j.sjpain.2016.08.002
Acknowledgement
We acknowledge with gratitude the patience of our study participants despite their adversaries of living with migraine especially in our resource limited setting. The authors also acknowledge the contributions of the nurses and medical record staff of FNPH Maiduguri. We also appreciate the intellectual contributions of Marco Lisicki while preparing the manuscript.
Declarations/Disclosures
Ethical Approval: Approval for the study was obtained from the Health Research and Ethics Committee (approval no: FNPH/032020/REC042), Federal Neuropsychiatric Hospital Maiduguri, Nigeria. The research was performed in accordance with the Declaration of Helsinki.
Consent/Permissions: All participants gave informed consent before taking part in the study.
Funding: None.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, author declares the following:
Payment/services info: Author has declared that no financial support was received from any organization for the submitted work.
Financial relationships: Author have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: Author have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
