Author: Lynn Kohan MD * 1, Samer Narouze MD PhD 2, Dmitri Souza MD PhD 3, M David Gothard MS 4, Scott Brancolini MD 5
Author Affiliation:
1 Associate Professor Anesthesiology and Pain Medicine, Director Pain Fellowship, Department of Anesthesiology and Pain Medicine, University of Virginia, Charlottesville, VA
2 Professor of Surgery and Anesthesiology, NEOMED Chairman, Center for Pain Medicine, Western Reserve Hospital, Cuyahoga Falls, OH
3 Director of Clinical Research, Western Reserve Hospital, Cuyahoga Falls, OH
4 Biostats Inc. East Canton, OH
5 Associate Professor Anesthesiology and Pain Medicine, Director Pain Fellowship, Department of Anesthesiology and Perioperative Medicine, University of Pittsburgh Medical Center, Pittsburgh, PA
Research Support: Support was provided solely from institutional and/or departmental sources.
Competing Interests: The author/s declare no competing interests.
Issue: 02.05
DOI: doi.org/10.30756/ahmj.2020.02.05
Received: April 8, 2020
Revised: April 11, 2020
Accepted: April 16, 2020
Published: April 21, 2020
Recommended Citation: Kohan L, Narouze S, Souza D, et al. Do Pain Medicine Fellowships Provide Adequate Education in Head and Facial Pain? A Survey of Pain Medicine Fellowship Program Directors. Ann Head Med. 2020;02:05. DOI: 10.30756/ahmj.2020.02.05
Background: Fellows with insufficient education in head and facial pain may feel ill equipped to treat patients suffering from these disabling disorders. We hypothesized that there is variation in the scope and extent of headache and facial pain education that pain fellows receive during their pain fellowship.
Study Design: A survey
Setting: Accreditation Council for Graduate Medical Education (ACGME) Accredited pain medicine fellowship programs.
Methods: After an exemption was obtained from the University of Virginia Institutional Review Board (IRB), an email with a link to the survey was sent to members of the Association of Pain Program Directors (APPD). The survey was also distributed to Association of Pain Program Director members at the annual 2019 APPD meetings during the Annual Society of Associations of Academic Anesthesiologists and Perioperative Medicine (SAAAPM) and the American Society of Regional Anesthesia and Pain Medicine (ASRA) meetings. The survey contained 16 questions. (questions are shown in Appendix 1).
Results: Forty-seven of 108 program directors responded to the survey. Some program directors did not respond to every question.
Limitations: The response rate is a limitation, but it is comparable to similar studies.
Conclusions: The majority of pain fellows receive some education in head and facial pain. However; there were variations among fellowship programs in the extent and scope of education provided. Recognizing these gaps and variations in education, may lead to a better understanding of how to enhance and provide head and facial pain education during pain fellowship.
Introduction
Trainees enrolled in pain medicine fellowships accredited by the ACGME must acquire a plethora of knowledge and skills in a one-year period. According to the ACGME, pain fellows are expected to receive education related to numerous pain conditions during this time including education about facial pain and headache disorders. Education can be provided in numerous formats including didactics, off-service neurology rotations, courses/workshops, direct observation during clinic or procedural management, as well by providing direct clinical care to patients with these disorders.
The World Health Organization (WHO) identifies headache disorders as the most common primary disorder of the nervous system 1, thus a large percentage of patients can be expected to suffer from this disabling condition. Socioeconomic costs associated with headache are estimated at $14 billion per year 2. Lifetime prevalence of headache is approximately 96% 3. Migraine headache alone impacts almost 15% of the population in the United States 4 and is associated with significant reports of impaired function. An astounding 50% of afflicted individuals report severe impairment limiting daily activities or requiring bed rest during a migraine attack 5. Tension headache also has a significant impact with an estimated prevalence of approximately 40% 3. Worldwide, the prevalence of chronic daily headache is consistently reported at 3-5% 3.
Despite the astounding prevalence and degree of impairment associated with headache disorders, numerous pain physicians refrain from treating this patient population. Studies have not been conducted to elucidate the cause of this hesitation. Headache disorders are often underestimated, under-recognized, and under-treated worldwide 6. It is suggested that only a minority of people with headache disorders are appropriately treated by a headache specialist 6. Globally, the WHO reports that only 4 hours of undergraduate medical education are dedicated to instruction on headache disorders 6. We hypothesize that inadequate education during fellowship training may predispose practicing physicians to refrain from treating this large patient population. We devised a survey for pain fellowship directors to gain understanding of the current head and facial pain curriculum being employed in pain fellowships in order to assess if current curriculums are adequately educating todays trainees.
Methods
The study was awarded IRB Review Exempt status by the University of Virginia IRB. A web-based survey was hosted by Qualtrics Inc. and sent via email with a survey link to program director members of the APPD at the end of the 2018-2019 academic year (June 13-June 30, 2019). Paper surveys were also distributed during the APPD Meetings at the annual SAAAPM and the Fall ASRA 2019 meetings. Participants were asked to not complete the survey more than 1 time. To create the survey, the key components of comprehensive head and facial pain diagnosis and treatment were identified by the primary author. The survey questions were then reviewed and revised by SN and DS, pain medicine and headache medicine specialists, to ensure clarity and comprehensiveness of all questions. The survey was then uploaded into Qualtrics and pretested with via cognitive interviews with all authors. In order to identify inconsistencies in the interpretation of the survey questions, the answers were collected and compared to one another. Questions were then adjusted to ensure the questions were perceived as intended, understood, and inclusive of all possibilities. The survey queried the extent and scope of education fellows receive in the diagnosis and treatment of head and facial pain disorders. In addition, the type of educational content utilized in the teaching was assessed. The survey also included demographic information such as location and size of fellowship (Appendix 1). Results were reported both as descriptive statistics and analyzed with Kendal’s tau for ordinal associations.
Results
Demographics
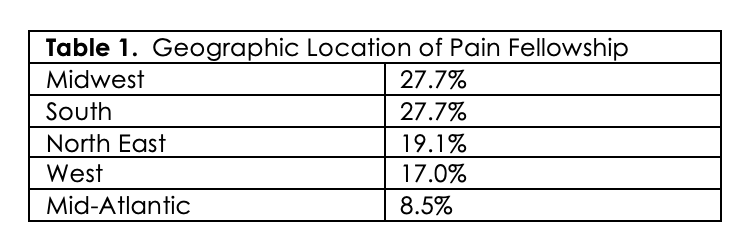
Forty-seven of 108 program directors (PDs) from ACGME-accredited pain fellowships responded to the survey (44% response rate). The majority of respondents indicated anesthesiology was their primary specialty (91.5%), followed by neurology (6.4%), and physical medicine and rehabilitation (2.1%). In regard to fellowship size, the majority of fellowship (48.9%) have 4-6 fellows, followed by 2-3 fellows (36.2%), 7-8 fellows (8.5%),1 fellow (4.3%), and > 8 fellows (2.1%). Respondents were also asked if the fellowship had board-certified headache attendings on staff. Sixty-six percent of fellowships do not have a board-certified headache specialist on staff. Geographic location of the fellowship was also assessed and can be viewed in Table 1.
Scope and Method of Education
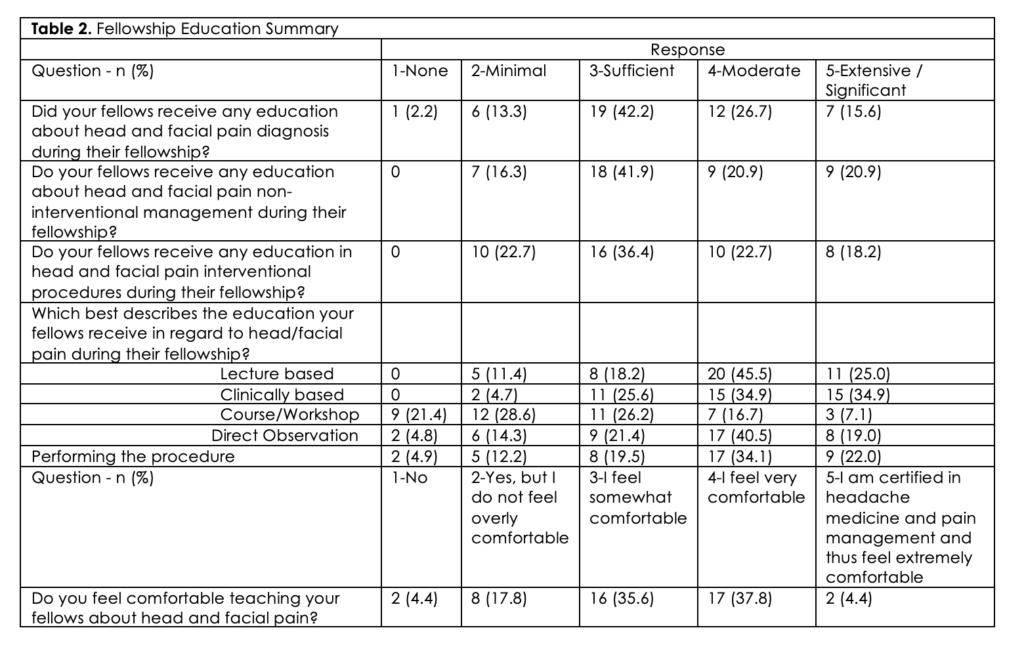
PDs were surveyed on the scope of head and facial pain education in their fellowships. Approximately 80% of programs reported they provided at least “sufficient” education in the diagnosis and treatment (both non-interventional and interventional) of headache and facial pain. In regard to teaching methods employed, lectures and clinical based education were “moderately” to “extensively” utilized in about 70% of programs and direct observation in about 50% of programs. Approximately 50% of program’s fellows received “minimal” or “no” education in the form of workshops or courses. Almost 20% of programs reported “minimal” to “no” use of direct performance of the procedure by the trainee as a form of education. Close to 60% of PDs reported that -at most- they felt “somewhat comfortable” teaching their fellows about head and facial pain. A summary of these findings is found in Table 2.
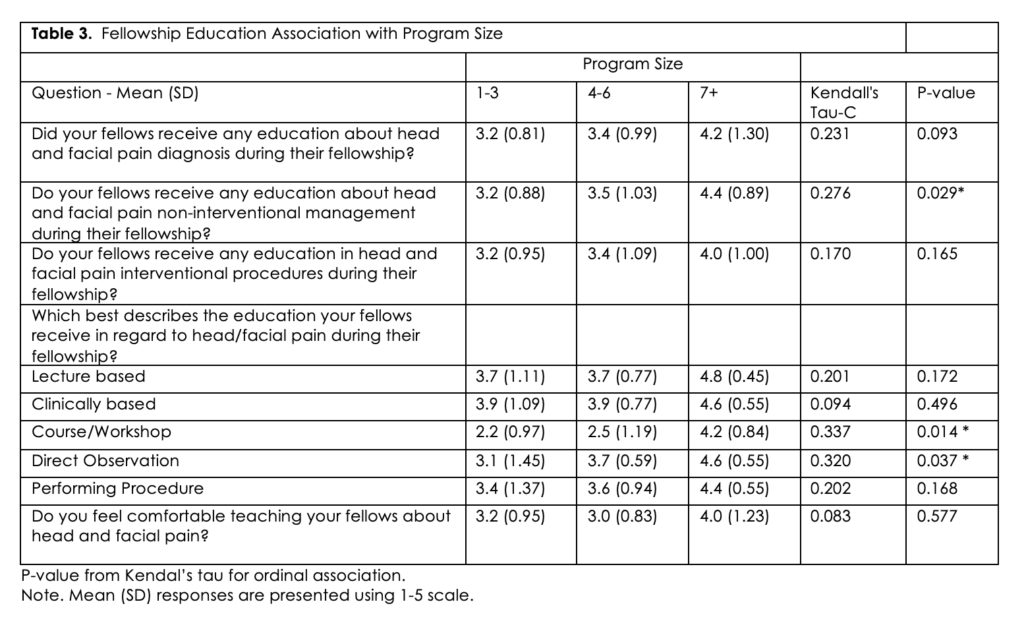
Data was also analyzed for the relationship between fellowship size and the extent and scope of head and facial pain education pain fellows receive. Results indicate a significant correlation between fellowship size and the scope of non-interventional head and facial pain fellows received with larger fellowships more likely to provide non-interventional education than smaller fellowships. In addition, larger fellowships were more likely to use courses/ workshops and direct observation to provide the education. There were no other significant differences in the scope or extent of education in comparison to fellowship size. (Table 3)
Educational Content (Headache Diagnosis, Medication Class, Interventional Technique)
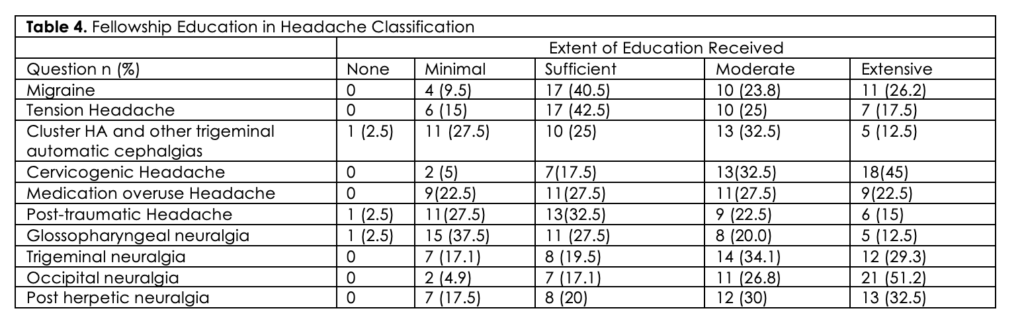
The survey also assessed the degree of education fellows received in different headache disorders, medication classes, and interventional procedures. The majority of programs (>75%), reported at least “sufficient” education in migraines, tension type headaches, cervicogenic headache, and occipital neuralgia. On the other hand, approximately one quarter of PDs indicated that their fellows received “minimal” to “no” education in medication overuse headaches (MOH), post-traumatic headache, and glossopharyngeal neuralgia. (Table 4)
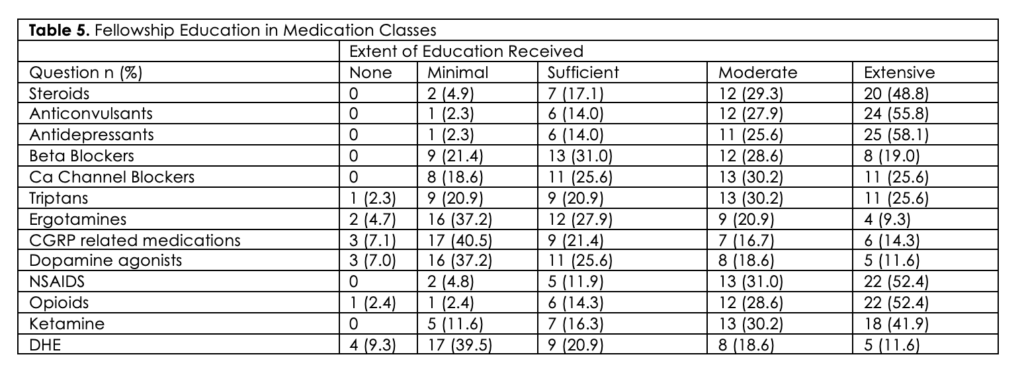
 For medication classes, almost 25% of PDs reported their fellows had “minimal” to “no” education in triptans, while almost half reported “minimal” to “no” education in ergotamine, calcitonin gene related peptide medications (CGRP), dopamine agonists, and dihydroergotamine (DHE). Most programs reported they provided at least “sufficient” education in the use of steroids, anticonvulsants, antidepressants, beta blockers, calcium channel blockers, non-steroidal anti-inflammatory drugs (NSAIDS), opioids, and ketamine in the treatment of headache disorders. (Table 5)
For medication classes, almost 25% of PDs reported their fellows had “minimal” to “no” education in triptans, while almost half reported “minimal” to “no” education in ergotamine, calcitonin gene related peptide medications (CGRP), dopamine agonists, and dihydroergotamine (DHE). Most programs reported they provided at least “sufficient” education in the use of steroids, anticonvulsants, antidepressants, beta blockers, calcium channel blockers, non-steroidal anti-inflammatory drugs (NSAIDS), opioids, and ketamine in the treatment of headache disorders. (Table 5)
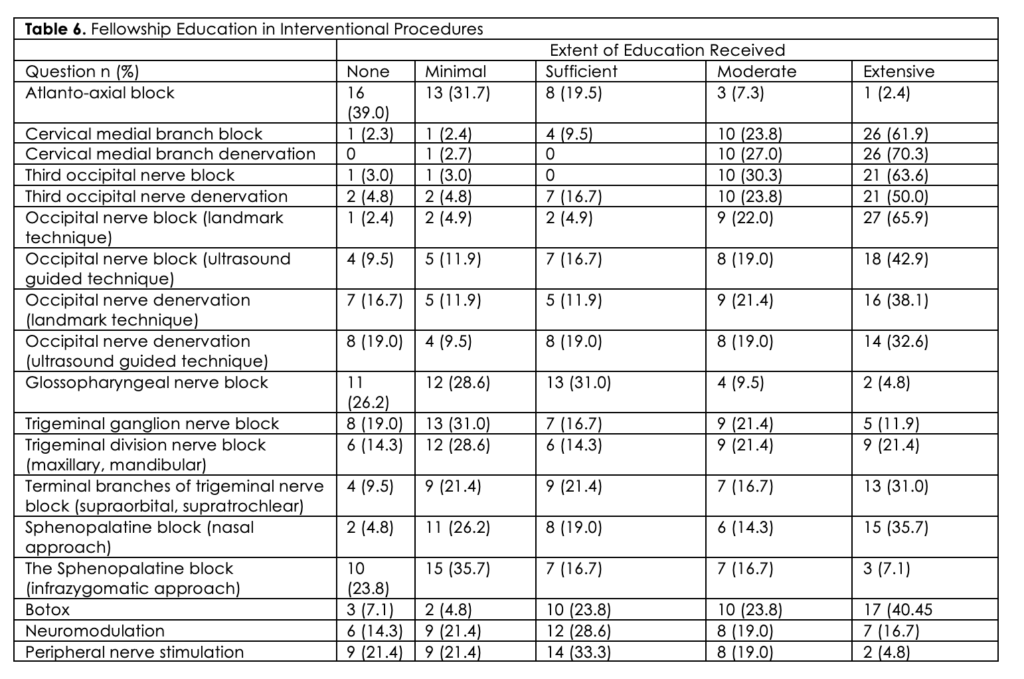
Seventy percent of PDs responded that their fellows had “minimal” to “no” exposure to atlanto-axial blocks. Approximately half of fellows had “no” or “minimal” education in glossopharyngeal blocks, trigeminal nerve blocks (including ganglion and nerve divisions), sphenopalatine nerve blocks (infrazygomatic approach), and peripheral nerve stimulation. Approximately 30% of fellows had “no” or “minimal” education in occipital nerve denervation using either landmark or ultrasound techniques, blocks of the terminal branches of trigeminal nerve (supraorbital, supratrochlear), sphenopalatine blocks (nasal approach), and neuromodulation techniques. Fellows in the majority of programs (>75%) received education in the use of cervical medial branch block, cervical medial branch denervation, third occipital nerve block, third occipital nerve denervation, occipital nerve block (landmark or ultrasound technique), and Botox for the treatment of head and facial pain disorders. (Table 6)
Discussion
Pain medicine fellows come from different backgrounds, therefore their prior exposure to head and facial pain education is highly variable, suggesting a need for a more structured curriculum within pain fellowships. Study results indicate that the extent and type of education fellows are provided during their fellowship varies. Variations existed in the degree of non-interventional and interventional training, type of educational format utilized by programs, and the extent of education fellows obtained in different head/facial pain disorders and treatments.
Scope and Method of Education
Over 15% of programs indicated their fellows did not receive at least sufficient overall education in head and facial pain. Sixteen percent of programs indicated fellows were not at least “sufficiently” educated in use of non-interventional treatment techniques, while one third reported the same regarding the use on interventional techniques. There was trend for larger programs to report providing a greater degree of overall headache education, however this finding was not statistically significant. When divided into non-interventional and interventional education, larger programs were statistically more likely to provide at least sufficient non-interventional education compared to smaller programs. There was no correlation between degree of interventional education and size of program. It is unclear why larger programs were more likely to provide non-interventional vs interventional education, however it can be speculated that perhaps they have more faculty/educational resources as well as higher volume and referrals to be able to do so or that fellows in these institutions were able to obtain education in well-developed neurology rotations as part of their off-site ACGME requirement.
Lecture and clinically based education were the most frequent resources employed in the training programs with all PDs reporting utilizing these methods and 70% relying on them moderately to extensively. About half of programs used direct observation and workshops/courses to teach fellows with larger programs being statistically more likely to use these methods than smaller programs. It is likely that larger programs have more resources to be able to provide courses/workshops than smaller programs. It is unclear why smaller programs were less likely to rely on direct observation than larger programs to teach head and facial pain treatment techniques. Twenty percent of PDs indicated that direct procedural care was not utilized as an educational method for their fellows. Larger and smaller fellowships did not differ in their utilization of this teaching method. The majority of PDs reported they felt at the most only “somewhat comfortable” teaching head and facial pain concepts to their fellows. This lack of comfort may be secondary to PDs themselves receiving inadequate training or experience during their own fellowships or career development in head and facial pain.
Headache disorders
The survey also examined the scope of education that fellows were receiving, including variations in education on different types of headache disorders. It is concerning that almost 25% of programs provided minimal to no education on migraines, tension type headaches, cervicogenic headache, and occipital neuralgia, as well as MOHs. Insufficient education on migraine, tension headaches, and MOH is of serious concern given the prevalence of these conditions world-wide, associated severe disability, and significant economic impact 1,3. These conditions cause significant impairment to patients’ daily lives.
Furthermore, while perhaps less prevalent, cervicogenic headache and occipital neuralgia, can also cause disabling pain with significant impact of patients’ quality of life. In regard to MOH, it has been estimated that up to 4% of the population overuse analgesics and other drugs for the treatment of pain conditions including migraine7. An older survey of family doctors reported that MOH was the 3rd most common aggravating factor contributing to the chronification of a pre-existing headache. Among headache clinics in North American, the incidence of MOH has been reported in up to 70% of patients8. More recent evidence suggests that MOH is a condition that affects about 60 million people worldwide, is among the top 20 causes of disability 9 and is associated with significant socioeconomic consequences 10. The associated costs (sick leave, lack of productivity, increased medication use, and frequent healthcare use) of MOH are actually 3 times higher than that of migraine 11. Furthermore, secondary to recall bias, diagnosing MOH may be challenging. In addition, other diagnoses in the International Classification of Headache Disorders 3rd Edition may be consistent with the described symptoms of MOH thus further contributing to diagnostic difficulties. Abortive medication overuse is a high-risk factor for migraine chronification and may significantly impair treatment efficacy. Therefore, its recognition and proper management may impact migraine prognosis and overall treatment outcome. Given MOH’s prevalence and associated morbidities, it is essential for providers to obtain adequate training in this disorder. Knowing the diagnostic complexity of the disorder, it might be assumed that the more education one receives in this disorder the better equipped the provider will be to diagnose and treat it. However, even brief educational interventions were found to have a significant impact. A study in Norway reported a 50% reversion in the incidence of chronic to episodic headache among patients whose general practitioners were given a 1-day introduction course to MOH. It appears that much can be done to strengthen the education provided in pain fellowships in this disorder to better equip todays pain fellows with the tools needed to curtail this epidemic.
An even higher percentage of PDs (approximately 1/3) reported their fellows had “minimal” to “no” education in trigeminal autonomic cephalalgias (TACs). While trigeminal autonomic cephalgias occur less frequently than other headache disorders, they can be especially debilitating, thus education in this field is essential. Evidence suggests that patients with (TACs) continue to suffer from delayed diagnosis and inappropriate treatment, despite being treated in secondary care clinics 12. A cluster headache survey in the US found that cluster headache (a type of TAC) patients experience on average a 5-year delay in diagnosis and only 21% receive a correct diagnosis on initial presentation 13. Furthermore, the severity of cluster headache disorder has major effects on patients’ quality of life, and in some cases can even lead to suicidal ideation 14, obviating a need for formal education in this disorder.
Similar to TACs about one third of PDs reported minimal to no education in post-traumatic headache (PTH) disorders. PTH disorder is also of important clinical significance. Headache is the most common symptom after a traumatic brain injury (TBI) with a reported incidence of 71% after moderate or severe TBI and an even higher incidence after mild TBI (91%) 15. PTH is often not well managed and self-treatment is often common. While treatment can be complex it is necessary to improve awareness/education of this condition to decrease the global burden and suffering from this condition.
Medications
We also studied the extent of medication management education pain fellows receive. Most consistency was reported among programs in providing education on the use of steroids, antiepileptics, antidepressants, NSAIDs, opioids, and ketamine with the majority of programs reporting at least “sufficient” education on these topics. However, there was wide variation in the extent of education on beta blockers, calcium channel blockers, triptans, ergotamines, CGRP related medications, dopamine agonists, and DHE.
Almost half of PDs (47.5%) reported providing “minimal” to “no” education on the use of CGRP related medication for the use of headaches. CGRPs are an exciting breakthrough for the treatment of migraine headaches. Previously the major turning point in the treatment of migraine had been the development of 5-HY1B/1D receptor agonists (triptans). Triptans were found to be efficacious in the treatment of acute migraine and its associated symptoms 16, however their use was limited secondary to associated cardiovascular risks17. Furthermore, only about 1/3 of patients obtained sustained relief from oral triptans (freedom of pain at 2 hours with no rescue medication and with no recurrence of headache within 24 hours) 18. Therefore, there was a need to develop medications with greater efficacy and with less adverse effects. CGRP has been indicated as playing a crucial role in the central and peripheral pathways leading to a migraine attack 19. Thus, these medications are emerging as novel treatment options for patients suffering from migraine. It is imperative that today’s pain fellows be provided education on the use of these emerging medications.
Almost 50% of PDs reported “minimal” or “no” education on DHE for their pain fellows. DHE was actually one of the first synthetic drugs developed in the 20th century for treating migraine. Oral DHE is extensively metabolized thus it should be given via a non-oral route. Intravenous DHE is commonly used but requires health-care providers to administer. It is likely that DHE is administered via the neurology service in most academic institutions thus limiting exposure to pain services. DHE is also available in subcutaneous/intramuscular formulations but may be challenging for patients to self-administer. The currently approved Food and Drug Administration nasal spray formulation has low bioavailability and high variability that limits its efficacy 20. While the administration of DHE may be more complicated than other migraine medications, it is still an effective treatment particularly for difficult to treat migraine with associated symptoms such as allodynia. Novel DHE agents are also being developed. Therefore, it is important for all pain physicians to be familiar with the use of DHE in the treatment of migraine and education on the use of this drug should be incorporated into more pain fellowship program curriculums.
Ketamine is also an emerging medication in the treatment of headache disorders. Most pain physicians are already familiar with its use for other pain disorders, such as complex regional pain syndrome. A recent retrospective analysis by Shwenk et al found that ketamine was associated with short-term analgesia and tolerable adverse effects in many patients with refractory headache21. Almost 90% of programs are incorporating education on the use of ketamine into their curriculums, suggesting that fellows are being adequately educated on the use of this drug.
Interventional treatments
Programs showed overall consistency in providing education for some interventional techniques while there was a wider variation found among other techniques. Procedures with the most consistency included cervical medial branch blocks/denervations, third occipital nerve, atlanto-axial nerve blocks, and use of onabotulinumtoxinA. A wider variation in education was noted for nerve blocks of the trigeminal nerve (ganglion, division, and terminal branches), glossopharyngeal nerve, and the sphenopalatine nerve (via either the nasal or infrazygomatic approach. Neuromodulation techniques appear to be an emerging technology in which fellows are receiving education.
A large degree of consistency was found in education for cervical medial branch blocks/denervations and third occipital nerve blocks (ONBs) with overall over 90% of programs teaching these techniques at least sufficiently. While consistency was noted in ONB education, variation existed regarding use of the blind/landmark technique versus ultrasound guidance when performing these procedures. More consistency existed in the use of these 2 modalities when performing ON denervation. The survey did not evaluate the etiology of these findings, but one may speculate that US was used more frequently for ON denervation in order to more precisely denervate the nerve given the smaller impacted area as opposed to use of a field block when performing an ONB.
Consistency was also noted in the use of atlanto-axial blocks with the majority of programs providing minimal to no education in this area. There are inherent risks involved when performing atlanto-axial blocks, therefore it is important to provide pain fellows education on this topic even if they are not performing the procedure during their fellowship.
Less consistency was noted for education on nerve blocks of the trigeminal nerve (ganglion, division, and terminal branches), glossopharyngeal nerve, and the sphenopalatine nerve (via either the nasal or infrazygomatic approach). Over 50% of programs reported providing “no” to minimal” glossopharyngeal or sphenopalatine (infrazygomatic approach) education. PDs and faculty likely have less education/training in these techniques themselves and thus are less likely to utilize them in their practice, impacting both fellows’ education as well as patient care. While glossopharyngeal neuralgia (GN) is a relatively rare condition, it is characterized by severe, paroxysmal episodes of pain localized to the external ear canal, base of the tongue, tonsil, or the area beneath the angle of the jaw 22. GN can often be misdiagnosed as trigeminal neuralgia (TN). Thus, education in proper diagnosis and treatment of GN and TN is paramount. The variation noted in these areas of education suggests a need to provide better resources to programs that are not currently utilizing these techniques or perhaps the creation of a uniform pain fellowship curriculum.
Consistency was also noted regarding education for onabotulinumtoxinA. The majority of programs (92.7%) report providing at least “sufficient” education in the use of onabotulinumtoxinA in the treatment of head and facial pain disorders. Chronic migraine (CM) is a severe and disabling condition impacting approximately 2-3% of the population 23. Patients with CM experience significant headache-related disability, reduced health-related quality of life, and co-morbidities 24. Treatment with onabotulinumtoxinA has been proven to be effective at reducing headache symptoms and improving health-related quality of life in patients with CM 25. It is therefore encouraging that a large percentage of pain fellows are obtaining education in the use of this medication.
Neuromodulation and peripheral nerve stimulation are emerging fields in the treatment of head and facial pain. There are both invasive and non-invasive treatment options, such as hypothalamic deep brain stimulation, occipital nerve stimulation, supraorbital nerve stimulation, stimulation of the sphenopalatine ganglion, cervical spinal cord stimulation, vagus nerve stimulation, and transcutaneous electrical nerve stimulation. These techniques have been used with success; however randomized controlled trials are ongoing 26. Our study found that a fair number of programs are providing education in these modalities. 64.1% of PDs reported providing education in neuromodulation and 57% in peripheral nerve stimulation. Given the novelty of this field, it is encouraging that PDs are incorporating this growing knowledge into their curriculums.
Limitations
There were several limitations to this study including the response rate. The survey also did not contain complete data regarding the primary specialty of the PD reporting his/her comfort level educating fellows about head and facial pain. Furthermore, it did not identify length of time the PD has been in practice nor the extent of education he/she had received in his/her own training or career development. The lack of this information could have impacted the results of the study as PDs whose core specialty was neurology or those with more extensive education in their fellowship or career development might have reported a higher level of comfort with head and facial pain syndromes and treatment. Furthermore, they survey did not ask about referral patterns. The extent and scope of direct clinical/procedural education provided can be impacted by referral patterns. Since pain fellowships are in academic institutions that often also have neurology departments with specialized headache clinics, pain fellows might have less access to patients suffering from head/facial pain. Thus, provider comfort is not the only impacting factor on the above findings.
Conclusion
Head and facial pain is a debilitating condition that impacts numerous patients. The patients impacted by this disorder often suffer for long periods of time while awaiting treatment either secondary to physician shortages or misdiagnosis from lack of education 6. The ACGME stipulates that pain fellows obtain education in a multitude of painful conditions including head and facial pain. Thus, pain physicians are in a unique situation to be able to treat this patient population, however it appears that there is a reluctance among pain physicians to do so. While referral patterns primarily to neurologists may certainly play a role, it does not appear that pain physicians are advocating to treat this patient population. While clear causes for this reluctance are unknown, lack of confidence or education in treating these conditions may play a role. The survey indicates that there appears to be variation among pain fellowships in the education that is received. Approximately one quarter of PDs indicated that their fellows received “minimal” to “no” education in medication overuse headaches (MOH), TACs, and migraine-specific medications. While almost 50% had minimal or no education in many interventional headache procedures and neuromodulation. Efforts should be undertaken to help standardize the education that fellows are obtaining in order to better equip our future pain physicians with the tools needed to care for this subset of patients. One step towards achieving this is to encourage pain physicians to seek headache board certification as our survey revealed that 66% of fellowships do not have a board-certified headache specialist on staff. Currently; there are 3 headache medicine certifications available for qualified physicians. They are offered through the United Council for Neurologic Subspecialties, the American Board of Headache Medicine, and the National Headache Foundation 27,28,29, none of which are members of the American Board of Medical Specialties. Certification can often be obtained by completing a course and/or examination. Striving towards these goals may allow for better care of this underserved patient population.
References
- Neurological Disorders Public Health Challenges. World Health Organization. Accessed 5/20/2019. PDF
- Hux H, Markson LE, Lipton RB, et al. Burden of migraine in United States: disability and economic costs. Arch Intern Med. 1999 Apr 26;159 (8): 813- 818. PubMed CrossRef
- Robbins MS, Lipton RB. The epidemiology of primary headache disorders. Semin Neurol. 2010 Apr;30(2):107-119. PubMed CrossRef
- Burch R, Rizzoli P, Loder E. The Prevalence and Impact of Migraine and Severe Headache in the United States: Figures and Trends From Government Health Studies. Headache. 2018 Apr;58(4):496-505. PubMed CrossRef
- Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007 Jan;68(5):343-9. PubMed CrossRef
- Headache Disorders. World Health Organization. Accessed 1/15/2020. URL
- Diener, HC, Limmroth V. Medication-overuse headache: a worldwide problem. Lancet. 2004 Aug;3(8):475-483. PubMed CrossRef
- Rapoport A, Stang P, Gutterman, et al. Analgesic rebound headache in clinical practice: data from a physician survey. Headache. 1996 Jan;36(1):14-19. PubMed CrossRef
- Vos T, Allen C, Arora M, et al. Global burden of disease collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016 Oct 8;388(10053):1545-1602. PubMed CrossRef
- D’Amico D, Grazzi L, Curone M, et al. Difficulties in work activities and the pervasive effect over disability in patients with episodic and chronic migraine. Neurol Sci. 2015 May; 36 Suppl 1: 9-11. PubMed CrossRef
- Linde M, Gustavsson A, Stover LJ, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012 May;19(5) 703-711. PubMed CrossRef
- Larner, AJ. Trigeminal autonomic cephalalgias: frequency in a general neurology clinic setting. J Headache Pain. 2008 Oct;9(5):325–326. PubMed CrossRef
- Rozen TD, Fishman RS. Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache. 2012 Jan;52(1):99-113. PubMed CrossRef
- Hoffman J, May A. Diagnosis, pathophysiology, and management of cluster headache. Lancet Neurol. 2018 Jan;17(1):75-83. PubMed CrossRef
- Lucas, S. Posttraumatic Headache: Clinical Characteristics and Management. Curr Pain Headache Rep. 2015;19:48. CrossRef
- Schulman EA, Dermott KF. Sumatriptan plus metoclopramide in triptan-nonresponsive migraineurs. Headache. 2003 Jul-Aug;43(7):729–33. PubMed CrossRef
- Papademetriou V. Cardiovascular risk assessment and triptans. Headache. 2004 May;44 Suppl 1:S31–9. PubMed CrossRef
- Goadsby PJ, Lipton RB, Ferrari MD. Migraine-current understanding and treatment. N Engl J Med. 2002 Jan;346(4):257–70. CrossRef
- Goldsberg S, Silberstein S. Targeting CGRP: A new era for migraine treatment. CNS Drugs. 2015 Jun;29(6):443-452. PubMed CrossRef
- Silberstein S, Shrewsbury S, Hoekman J. Dihydroergotamine (DHE)-then and now: a narrative review. Headache. 2020 Jan;60(1):40-57. PubMed CrossRef
- Shwenk E. Dayan A, Rangavaijula A, et al. Ketamine for refractory headache: a retrospective anaylsis. Reg Anes Pain Med. 2018 Nov;43(8):875-879. PubMed CrossRef
- Singh PM, Kaur M, Trikha A. An uncommonly common: Glossopharyngeal neuralgia. Ann Indian Acad Neuol. 2013 Jan;16(1):1-8. PubMed CrossRef
- Barbanti P, Egeo G, Aurilia C, Piroso S. Rationale for use of onabotulinumtoxin A (Botox) in chronic migraine. Neuro Sci. 2015 May;36 Suppl 1:29-32. PubMed CrossRef
- Frampton J. Onabotulinumtoxin A (Botox): a review of its use in the prophylaxis of headaches in adults with chronic migraine. Drugs. 2012 Apr;72(6):825-845. PubMed CrossRef
- Diener HC, Dodick DW, Aurora SK, et al. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalalgia. 2010 Jul;30(7):804–14. PubMed CrossRef
- Martelletti P, Jensen R, Antal A, et al. Neuromodulation of chronic headaches: position statement from the European Headache Federation. J Headache Pain. 2013 Oct 21;14:86. PubMed CrossRef
- Headache Medicine Certification Through United Council for Neurologic Subspecialties. Accessed 4/6/2020. URL
- Headache Medicine Certification Through American Board of Headache Medicine. Accessed 4/6/2020. URL
- Certificate of Added Qualification (CAQ) in Headache Medicine from the National Headache Foundation through The National Headache Foundation. Accessed 4/6/2020. URL
Appendix 1
Program Director’s Headache and Facial Pain Survey
Q1 Please identify your primary specialty
- Anesthesiology
- Physical Medicine and Rehabilitation
- Neurology
- Psychiatry
- Non-core specialty
Q2 What is the geographical location of your fellowship
- Northeast
- Mid-atlantic
- South
- West
- Midwest
Q3 Please indicate the number of fellows in your fellowship
- 1
- 2-3
- 4-6
- 7-8
- >8
Q4 Are there any attendings that are board certified in headaches in your fellowship?
- Yes
- No
Q5 Do you have a board-certified neurologist on your faculty?
- Yes
- No
Q6 Is the neurologist also an interventionist?
- Yes
- No
Q7 Do you rely on that neurologist to teach about head and facial pain?
- Yes
- No
Q8 Do your fellows receive any education about head and facial pain diagnosis during their fellowship?
- None
- Minimal
- Sufficient
- Moderate
- Significant
Q9 Do your fellows receive any education about head and facial pain non-interventional management during their fellowship?
- None
- Minimal
- Sufficient
- Moderate
- Significant
Q10 Do your fellows receive any education in head and facial pain interventional procedures during their fellowship?
- None
- Minimal
- Sufficient
- Moderate
- Significant
Q11
Do your fellows receive education in the following during their fellowship?
| Please indicate the amount of education your fellows receive | |||||
| None | Minimal | Sufficient | Moderate | Extensive | |
| Migraine | o | o | o | o | o |
| Tension Headache | o | o | o | o | o |
| Cluster HA and other trigeminal autonomic cephalgias | o | o | o | o | o |
| Cervicogenic HA | o | o | o | o | o |
| Medication overuse headache | o | o | o | o | o |
| Post-traumatic headache | o | o | o | o | o |
| Glossopharyngeal neuralgia | o | o | o | o | o |
| Trigeminal neuralgia | o | o | o | o | o |
| Occipital neuralgia | o | o | o | o | o |
| Post-herpetic neuralgia | o | o | o | o | o |
Q12 Do your fellows receive education in the following during their fellowship?
| Please indicate the amount of education your fellow receives | |||||
| None | Minimal | Sufficient | Moderate | Extensive | |
| Steroids | o | o | o | o | o |
| Anticonvulsants | o | o | o | o | o |
| Antidepressants | o | o | o | o | o |
| Beta blockers | o | o | o | o | o |
| Ca Channel blockers | o | o | o | o | o |
| Triptans | o | o | o | o | o |
| Ergotamines | o | o | o | o | o |
| CGRP related medications | o | o | o | o | o |
| Dopamine antagonists | o | o | o | o | o |
| NSAIDS | o | o | o | o | o |
| Opioids | o | o | o | o | o |
| Ketamine | o | o | o | o | o |
| DHE | o | o | o | o | o |
Q13 Do your fellows receive education in the following during their fellowship?
| Please indicate how much experience fellows receive | |||||
| None | Minimal | Sufficient | Moderate | Extensive | |
| Atlanto-axial joint block | o | o | o | o | o |
| Cervical medial branch block | o | o | o | o | o |
| Cervical medial branch denervation | o | o | o | o | o |
| Third occipital nerve block | o | o | o | o | o |
| Third occipital nerve denervation | o | o | o | o | o |
| Occipital nerve block (Landmark technique) | o | o | o | o | o |
| Occipital nerve block (Ultraound-guided technique) | o | o | o | o | o |
| Occipital nerve denervation (Landmark technique) | o | o | o | o | o |
| Occipital nerve denervation (Ultrasound-guided technique) | o | o | o | o | o |
| Glossopharyngeal nerve block | o | o | o | o | o |
| Trigeminal ganglion nerve block | o | o | o | o | o |
| Trigeminal division nerve block (maxillary, mandibular) | o | o | o | o | o |
| Terminal branches of trigeminal nerve block (supraorbital, supratrochlear) | o | o | o | o | o |
| Sphenopalatine block (nasal approach) | o | o | o | o | o |
| Sphenopalatine block (infrazygomatic approach) | o | o | o | o | o |
| Botox | o | o | o | o | o |
| Neuromodulation | o | o | o | o | o |
| Peripheral nerve stimulation | o | o | o | o | o |
Q14 What best describes the education your fellows receive in regard to head/facial pain during their fellowship?
| Please indicate how much experience fellows receive | |||||||
| None | Minimal | Sufficient | Moderate | Extensive | Answer 2 | ||
| Lecture based | o | o | o | o | o | o | |
| Clinically based | o | o | o | o | o | o | |
| Course/workshop | o | o | o | o | o | o | |
| Direct observation | o | o | o | o | o | o | |
| Performing procedure | o | o | o | o | o | o | |
Q15 Do you feel comfortable teaching your fellows about head and facial pain?
- No, I do not feel comfortable.
- Yes, but I do not feel overly comfortable
- I feel somewhat comfortable
- I feel very comfortable
- I am certified in headache medicine and pain management and thus feel extremely comfortable
Q16 What do you identify as barriers in head and facial pain education?
- Not enough time to teach in a one-year fellowship
- There are no faculty in my dept/division that are comfortable with this subject
- The neurology rotation does not adequately address this topic
- I do not feel it is important to teach
- We do not get enough referrals for these patients (do not see them in our clinic)
Disclosures
Dr. Samer Narouze is the current EIC for Annals of Headache Medicine. Dr. Alexander Feoktistov was the acting EIC handling this manuscript.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: Lynn Kohan MD is a board member of the American Interventional Headache Society (AIHS), Samer Narouze MD is the Chairman of the Board and Founder of AIHS, and Dmitri Souza MD is the Treasurer of the AIHS.
This article adheres to the CARE guidelines as outlined by EQUATOR.
