Author: Esme Fuller-Thomson * MSW, PhD 1,2,3, Marta Sadkowski BA&Sc, BScN 1
Author Affiliation:
1 Institute for Life Course & Aging, University of Toronto, Toronto, Canada
2 Factor-Inwentash Faculty of Social Work, University of Toronto, Toronto, Canada
3 Cross-appointed to Faculties of Medicine & Nursing, University of Toronto, Toronto, Canada
Competing Interests: The author/s declare no competing interests.
Issue: 05.02
DOI: 10.30756/ahmj.2021.05.02
Received: Jan 25, 2020
Revised: May 11, 2021
Accepted: May 22 , 2021
Published: Jun 16, 2021
Recommended Citation: Fuller-Thomson E, Sadkowski M. Flourishing Despite Migraines: A Nationally Representative Portrait of Resilience and Mental Health among Canadians. Ann Head Med. 2021;05:02. DOI: 10.30756/ahmj.2021.05.02
Objective
1) To examine the relationship between migraine status and complete mental health (CMH) among a nationally representative sample of Canadians; 2) To identify significant correlates of CMH among those with migraine.
Methods
Secondary analysis of the nationally representative Canadian Community Health Survey – Mental Health (CCHS-MH) (N=21,108). Bivariate analyses and a series of logistic regression models were performed to identify the association between migraine status and CMH. Significant correlates of CMH were identified in the sample of those with migraine (N=2,186).
Results
Individuals without a history of migraine had 72% higher odds of being in CMH (OR=1.72; 95% CI=1.57, 1.89) when compared with those with a history of migraine. After accounting for physical health and mental health problems, the relationship between migraine status and CMH was reduced to non-significance, with both groups having an approximately equal likelihood of achieving CMH (OR=1.03; 05% CI=(0.92, 1.15). Among those with migraine, factors that were strongly associated with CMH were a lack of a history of depression, having a confidant, and having an income of $80,000 or more.
Conclusion
Clinicians and health care providers should also address co-occurring physical and mental health issues to support the overall well-being of migraineurs.
Introduction
The prevalence of negative mental health outcomes including suicidal thoughts and attempts is much higher among those with migraines 1-6. As demonstrated by a recent meta-analysis, migraine is linked to increased prevalence of mood, anxiety, and personality disorders, post-traumatic stress disorder (PTSD), and substance misuse co-occurring with PTSD or depression 1. In particular, mood and anxiety disorders are estimated to be between two and three times more prevalent among individuals with migraine than those without this condition 1. Moreover, migraineurs with a comorbid psychiatric disorder experience significantly greater headache-related disability and diminished quality of life compared to migraineurs without psychiatric comorbidities 7. Psychiatric comorbidities may also be associated with poorer prognosis and clinical outcomes 1. For example, individuals with migraine and depression may have a greater risk of disease progression from episodic to chronic migraine 8.
Historically, mental health has been interpreted as the absence of mental illnesses, such as depression and anxiety, or other indicators of mental distress, such as suicidal ideation 9. Mental health researchers are increasingly shifting toward a positive psychology paradigm, informed by Keyes’ two continua model of mental health and illness 10. Keyes conceptualizes mental health as a set of positive emotional, psychological, and social elements that exist along a continuum 11. Complete mental health (CMH) is conceptualized as a state in which an individual experiences flourishing mental health and the absence of mental illnesses 11, 12. For migraineurs, achieving CMH indicates significant resilience to the adverse mental health outcomes associated with the condition. To our knowledge, the relationship between migraine and CMH has yet to be investigated.
The goals of our study are twofold: first, we investigate the independent association between migraine and CMH in a population-based sample of Canadians. Second, using a subsample of Canadians with migraine, we develop a profile of the sociodemographic, health, and psychosocial characteristics of migraineurs who have achieved CMH. In our investigation of migraine and CMH, we consider a number of relevant variables that may help explain the relationship. These variables are reviewed briefly below.
Socioeconomic Variables
Measures of socioeconomic status are essential to consider given that migraine is negatively associated with both household income 13 and educational level 14, 15. Socioeconomic status is also associated with CMH; Canadians in the lowest income quintile are significantly less likely to be flourishing than Canadians in the high-middle and highest quintiles 16.
Health-Related Variables
Several health behaviors may be associated with migraine and mental health status, including higher body mass index (BMI) 17, 18 and smoking 19, 20. A number of health outcomes are also linked to both migraine and mental health, including chronic pain 21, insomnia 3, and limitations in instrumental activities of daily living (IADLs) 11, 22.
Psychosocial Variables
The prevalence of migraine is higher among individuals who are divorced, or single compared to those who are married 23, while married individuals are more likely than those who are widowed, separated, divorced, or single to experience CMH 16. Additionally, individuals with poor social support have a higher prevalence of migraine and recurrent headaches than individuals with adequate social support 23. Finally, those with migraines are more likely to report adverse childhood experiences (ACEs) 24 including physical abuse 25-28, sexual abuse 25, 27, and/or exposure to parental domestic violence 29 than those without migraines. In turn, ACEs are associated with loneliness, stress 30, lower mental wellbeing 31, and lower life satisfaction 30-32.
Positive Coping Strategies
There are various strategies that migraineurs may use to cope with their condition. Religious coping is a commonly used mechanism to cope with chronic pain 33. Overall, religious, and spiritual coping is generally associated with positive mental and physical health outcomes among those with chronic pain 34. However, relying on religious or spiritual coping in lieu of seeking medical support, or using negative religious coping, such as seeing pain as punishment, can lead to poorer long-term outcomes 34.
Some migraineurs may use physical activity as a coping strategy. A recent review on the association between migraine and physical exercise found that exercise can have a prophylactic effect for some migraineurs, potentially reducing the frequency, duration, and/or intensity of migraines 35. However, some research has found that exercise can trigger or aggravate migraines for certain migraineurs, specifically high intensity exercise or exercise with insufficient warm-up 35, 36.
Methods
As has been described elsewhere 6, 37-42, the present study utilized data from the 2012 Canadian Community Health Survey-Mental Health (CCHS-MH). The CCHS-MH is a cross-sectional nationally representative survey of the Canadian population, age 15 or older, living in the 10 provinces with an overall response rate of 68.9% 43. The CCHS-MH assesses the mental health status of Canadians and examines the links between mental health and social, demographic, geographic, and economic variables 43.
Ethical Approval Information
Institutional Review Board Approval was not required from the University of Toronto because this paper was based upon analysis of the CCHS-MH, which is a public use data set in which all information has been anonymized. Statistics Canada (the Canadian equivalent of the US Census Bureau) conducted the original data collection, and they obtained informed consent from all participants at the time the original data were collected.
Sample
The present study utilized two sub-samples of the full CCHS-MH. The first subsample is comprised of those respondents with complete data on migraine and mental health, in addition to each of the independent measures examined in the current study (n = 21,108). This sample was utilized to compare those with and without migraine, and the relationship between migraine status and CMH. The second subsample, made up of individuals who reported that they had been diagnosed with migraine by a health professional (n = 2186), was used to identify factors associated with CMH, specifically among those who have been diagnosed with migraine.
Measures
Migraine Status
Migraine status was assessed in the CCHS-MH by first asking the respondents if they had any “conditions diagnosed by a health professional” which are “expected to last or have already lasted 6 months or more.” Migraine was included as an option for potential health conditions and assessed using the question: “Do you have any migraine headaches?” 43.
Complete Mental Health
The outcome variable examined in this study was CMH and was measured as a binary variable comprised of three elements: (1) the absence of mental illness or substance dependence in the past year (i.e. depressive episode, anxiety disorders, bipolar disorders, alcohol and drug dependence, suicidal ideation). These variables were derived from the World Health Organization version of the Composite International Diagnostic Interview (WHO-CIDI), a structured diagnostic interview that generates diagnoses according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) and the International Classification of Diseases (ICD-10); (2) emotional well-being (i.e. happiness or life satisfaction); and (3) social and psychological well-being. The latter two elements were assessed using the Mental Health Continuum – Short Form (MHC-SF); 44. The MHC-SF measures dimensions of positive mental health, including emotional well-being (e.g. during the past month, how often did you feel happy and/or satisfied with your own life?), social well-being (e.g. during the past month, how often did you feel that you had something important to contribute to society?), and psychological well-being (e.g. during the past month, how often did you feel that you liked most parts of your personality? 44, 45. The psychometric properties of the MHC-SF have been well established 44. Individuals were classified as being in “complete mental health” if they reported at least 1 of the 2 measures of emotional well-being (i.e. happiness and/or life satisfaction in the past year) and at least 6 of the 11 measures of psychological and/or social wellbeing ‘every day’ or ‘almost every day’ during the past month in conjunction with the absence of any of the above listed forms of mental illness in the past year. For more information, refer to Statistics Canada 45.
Demographic Variables
This study included several relevant demographic covariates such as age (in decades), sex (self-reported male and female), self-identified race/ethnicity (Non-Aboriginal White vs Visible Minority which includes Aboriginal), highest level of achieved education (less than post-secondary diploma or university degree versus post-secondary or higher), and total household income.
Adverse Childhood Experiences
Multiple childhood stressors were examined including childhood physical abuse, childhood sexual abuse, and exposure to chronic parental domestic violence. Childhood physical abuse was measured as a binary variable based on whether or not respondents had been kicked, bitten, punched, choked, burnt, or physically attacked by an adult at least once before age 16. Childhood sexual abuse was a binary variable indicating if participants indicated that an adult forced or attempted to force them into unwanted sexual activity at least once versus never. Chronic exposure to parental abuse was measured based on whether they reported having seen or heard 11 or more times one of their “parents, step-parents or guardians hit each other or another adult” aged 18 or over in their home 43. Socioeconomic factors examined include a dichotomous variable on post-secondary graduation and categorical annual household income level (<$20,000, $20,000–$39,999, $40,000–$59,999, $60,000–$79,999, $80,000 or higher).
Social Support Variables
Social support variables included marital status (married/ common-law vs single/divorced) and presence of a confidant. The latter variable was based upon the question “There is someone I could talk to about important decisions in my life” (strongly agree/agree vs disagree/strongly disagree).
Health Behaviors
Using a derived variable from Statistics Canada 43, smoking status was assessed in three categories: never smoked, former smoker and current smoker. Obesity was also categorized into three groups: a body mass index (BMI) of 30 or higher versus less; and a missing category. The BMI was calculated from self-reported weight and height.
Comorbid Health Conditions
Several comorbid health characteristics were included in this analysis. Insomnia was based upon the question “How often do you have trouble going to sleep or staying asleep?” (most or all of the time vs none/a little/some of the time). Debilitating pain was based on two questions: 1) “Are you usually free of pain or discomfort” (no/yes); and 2) “How many activities does your pain or discomfort prevent?” (none, a few, some, most). A combined dichotomous variable was created indicating the respondent had no pain or discomfort or, if they had pain, whether their activities were not limited by it versus those who reported their activities were limited by pain. Disability was assessed by asking the respondent “In the last 30 days, how much difficulty did you have in taking care of your household responsibilities?” (none/mild versus moderate/severe).
Mental Health History
Lifetime depressive disorders and lifetime generalized anxiety disorders were assessed for the WHO-CIDI lifetime criteria for each disorder. These scales are valid and reliable with a concordance between clinical interviews of 0.73 for anxiety/phobic disorders and 0.78 for depressive disorders 46. Wittchen 46 concluded that the test-retest and inter-rater reliability of these scales exceeds 90%.
Positive Coping Strategies
We also included in the analysis two distinct factors associated with better mental health outcomes in previous research: religion/spirituality and physical activity level. Religious coping was measured by asking respondents the extent to which spiritual or religious beliefs provide them with the “strength to face everyday difficulties” (some, a little or a lot versus not at all). Physical activity level was based on the number of times participants spent doing vigorous or moderate physical activity for leisure within the past 7 days (coded inactive, low activity, moderate or high activity).
Statistical Analyses
Using chi-square tests and independent t-tests in the full sample of Canadian community dwelling adults (n = 21,108), we compared and contrasted the profile of those with migraine (n = 2,186) to those without (n = 18,922). We then conducted a series of logistic regression analyses with CMH as the outcome. In the first and all subsequent models, we included migraine status. Model 2 included gender, race and age. Model 3 included the three adverse childhood experiences: physical abuse, sexual abuse, and exposure to parental domestic violence. Model 4 included marital status and confidant availability. Model 5 included smoking status and obesity. Model 6 included insomnia, self-rated physical health and difficulties with daily tasks. Model 7 included both physical activity and religious coping. Model 8 included lifetime history of depression and anxiety. Model 9 included all the variables listed above. In the subsample of the 2,186 who had migraines, a logistic regression analysis was included using all the variables in Model 9 above. All data were weighted to adjust for the probability of selection and non-response; however, sample sizes are reported in their original, unweighted form. Analyses were conducted using SPSS Statistics version 23.
Results
Adults with migraine had significantly lower prevalence of CMH than adults without migraine (63% vs 74%) (Please see Table 1). Those with migraine were younger and had a significantly higher prevalence of exposure to each of the three adverse childhood experiences than those without migraines. They also were more likely to have incomes under $20,000 per year and to be without a confidant than those without migraines. Migraineurs also were more likely to be a current smoker, to experience insomnia, debilitating pain, to have difficulties managing household activities, to be less physically active and to have a lifetime history of major depressive disorders and generalized anxiety disorders.
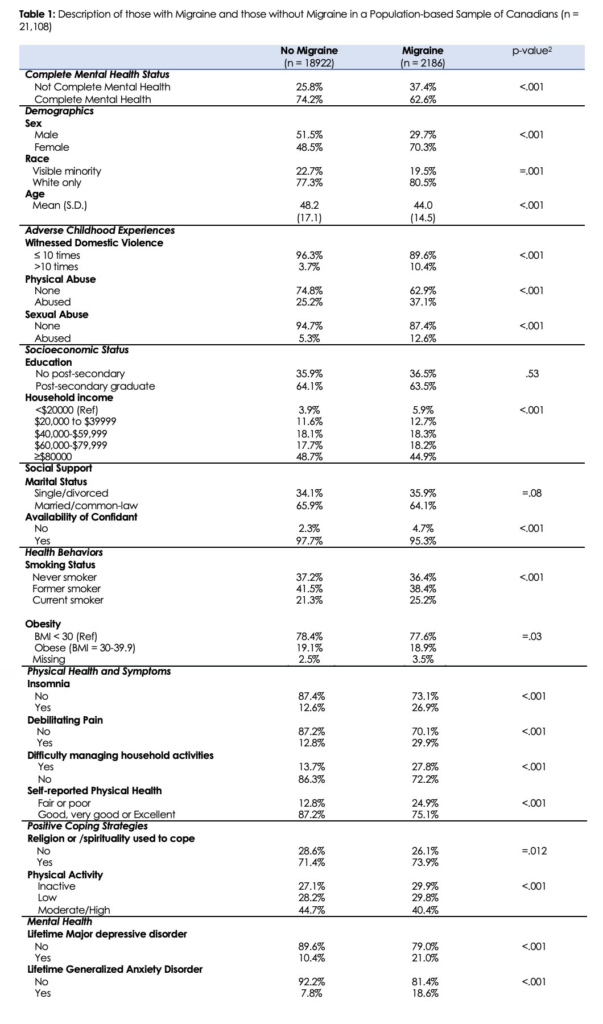
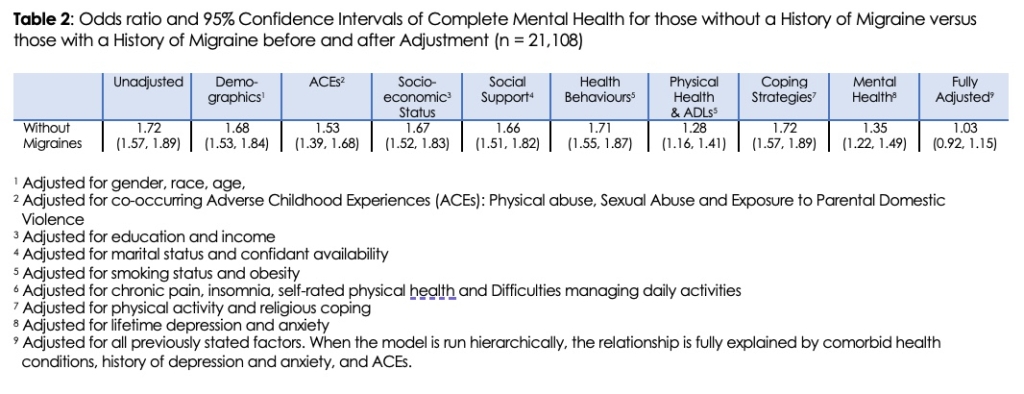
Table 2 presents the association between migraine history and CMH with a series of logistic regression models, each of which control for demographic covariates, as well as a cluster of potential explanatory factors. The unadjusted analysis indicated that adults without migraines had 72% higher odds of CMH when compared to those with migraines (OR=1.72; 95% CI=1.57, 1.89). Adjustment for demographic covariates, ACEs, socioeconomic status, social support, health behaviors and coping strategies did little to attenuate the association between migraine status and CMH (adjusted ORs range from 1.53 to 1.72). However, adjustment for chronic pain, insomnia, self-rated physical health and difficulties managing daily activities reduced the odds ratio by more than half (OR=1.28; 95% CI=1.16, 1.41), as did adjustment for lifetime history of depression and anxiety disorders (OR=1.35; 95% CI=1.22, 1.49). When all the above factors were combined together, the odds ratio was reduced to non-significance (OR=1.03; 95% CI=0.92, 1.15).
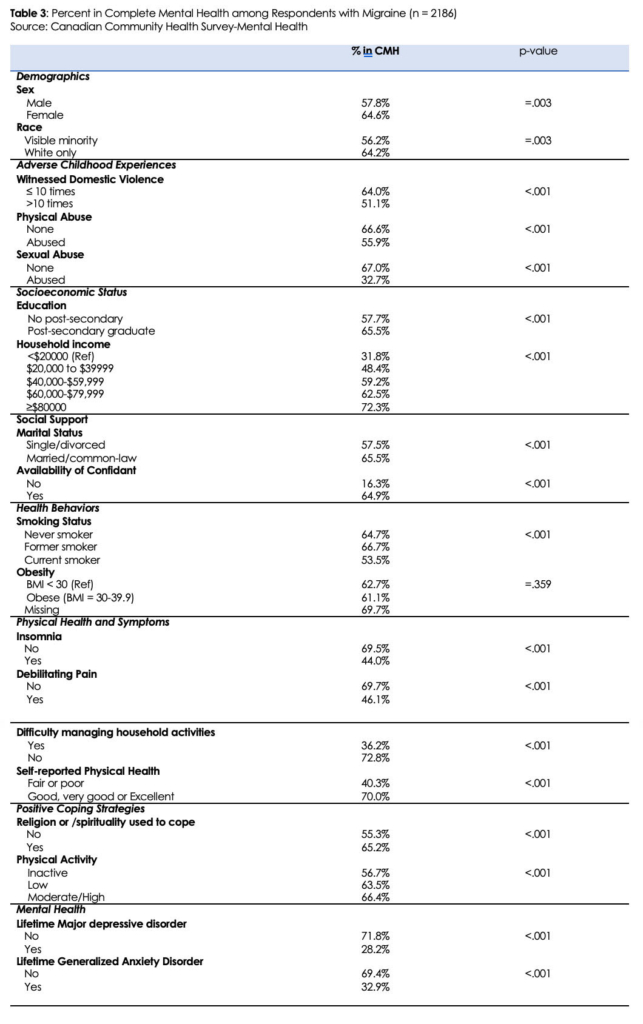
In addition to examining how migraine status relates to CMH, we also wanted to identify factors associated significantly with CMH in a sample of those with migraine (N=2,186). Those with migraine who were in CMH were slightly older (44.5, SD=14.7) than those who were not in CMH (43.1, SD=14.1; p=.03). As shown in Table 3, factors positively associated with CMH among those with migraine include being female, married, being white, having a confidant, reporting good or excellent health, and using spirituality to cope. The prevalence of CMH was lower among the physically inactive, adults who had experienced physical abuse, sexual abuse or chronic parental domestic violence during childhood, those whose household income was less than $20,000 per year, respondents who had difficulty managing their daily household activities, current smokers, and those who had ever been diagnosed with a major depressive disorder or anxiety disorders.
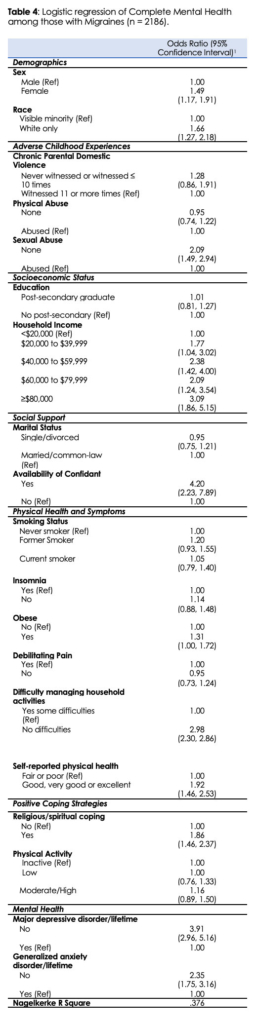
In a model adjusting for all factors simultaneously, the three most important correlates of CMH among migraineurs were having a confidant (OR=4.20), lack of a history of depression (OR=3.91) and having an income of $80,000 or more (OR=3.09). Other statistically significant correlates of CMH from the fully adjusted model include female gender, white race, lack of disability, having an income of at least $20,000, lack of a history of anxiety, having no difficultly managing household activities, use of religious coping, good self-rated health, and not having a history of sexual abuse.
Discussion
Our study is the first of which we are aware to investigate the relationship between migraine and CMH in a nationally representative sample. Our results indicate that while migraine status is significantly associated with a reduced likelihood of achieving CMH, this relationship can be explained by a history of poor mental health and the presence of health problems such as pain, insomnia, and IADL limitations. Once accounting for these covariates, those with migraine are as likely to achieve CMH as those without this condition. Given the high bar for achieving CMH and the numerous adverse mental health outcomes associated with migraines, the present study indicates substantial resilience among many migraineurs. This finding has important clinical implications for providing treatment to those with migraine.
First, it is essential to address co-morbid depression and anxiety when providing care to those with migraine. Individuals with migraine are significantly more likely to have anxiety, depression, or both mental conditions than those without migraine 47. The relationships between migraine, depression, and anxiety are likely bidirectional, with both mental conditions increasing the risk for migraine and vice-versa 47-49. The interrelationships between anxiety, depression, and migraine suggest shared etiological mechanisms 50, which may guide the development or selection of treatments for individuals presenting with these conditions. Several therapies have been shown to be effective in treating migraine and co-occurring depression and anxiety, including medications such as tricyclic antidepressants (e.g., amitriptyline 50, 51), and psychological treatments, such as biofeedback 52, 53, and cognitive behavioral therapy (CBT) 51
It is also important to consider how a shared underlying etiology may influence the relationship between migraine and chronic pain conditions, such as fibromyalgia 54. Some argue that these conditions may be collectively classified as “affective spectrum disorders” – a group of psychiatric and physical conditions that share specific but unknown etiological components including mitochondrial dysfunction, inflammation, and neurodegeneration 54. Future research into affective spectrum disorders may help in developing therapies that address the symptoms and underlying causes of migraine, as well as its comorbidities, which may improve clinical and psychosocial outcomes.
Our research also emphasizes the importance of treating the symptoms of migraine, such as pain, insomnia, and IADL impairments, to help individuals achieve CMH. Several therapies exist for managing migraine-related pain and co-occurring pain conditions, including medications (e.g., topiramate, botulinum toxin type A, sumatriptan 22), and psychosocial therapies such as biofeedback and CBT, which have been shown to reduce the frequency and severity of episodic migraine attacks, and may help individuals to develop pain management strategies 55.
Migraine is also associated with several impairments that may hinder IADL performance including fatigue, reduced vitality, and global disability 22. Prophylactic and symptomatic medications may help treat these migraine symptoms 22, however future research is required to further investigate the efficacy of these treatments for improving IADL performance in migraineurs.
In treating insomnia in those with migraine, clinicians should recognize that there is considerable overlap between coping behaviors used by individuals who experience headaches and perpetuating behavioral factors linked to chronic insomnia such as napping and caffeine use 56. Further research should examine whether CBT approaches used for treating insomnia in the general population can be adapted for migraine populations. It has been noted that migraine and insomnia often occur within a constellation of co-occurring physical and mental conditions such as fatigue, stress, and anxiety 3. Uhlig and colleagues 3 describe these co-occurring conditions as “syndrome-like”, meaning that they may share underlying etiological components. Given the complex etiologies of migraine and its associated comorbidities, broad interventions that target multiple symptoms or etiological components of these conditions may be pertinent for addressing these often-co-occurring issues.
There is a growing body of evidence that suggests a positive correlation between physical activity and both mental wellbeing 57 and life satisfaction 58. Regular exercise is also linked to a decreased probability of current major depression and anxiety disorders 59. Some evidence also suggests that exercise may decrease the number of migraine episodes per month, as well as episode severity in migraineurs 60. However, for some individuals, routine physical activity can also aggravate migraines 61. Further research is needed to investigate the efficacy of exercise in supporting CMH among individuals with migraine.
Our study makes a substantial contribution to the current literature by developing a profile of the health and psychosocial characteristics of migraineurs. While several studies have investigated correlates of CMH within other populations, such as those with depression 62, anxiety 63, suicidal ideation 64, stroke 65, and cancer 39 the present study is the first study, to our knowledge, to focus specifically on migraineurs.
Our results demonstrate that one of the strongest correlates of CMH in a population of migraineurs is history of depression, and furthermore, that within the general population, depression is strongly associated with increased odds of migraine. This relationship may be partially explained by the high levels of social isolation among migraineurs as a result of their difficulty with maintaining social and family relationships 66. Migraineurs often have a tendency to self-isolate as a coping strategy for uncontrollable migraine symptoms 67. Although the vast majority of migraineurs in the present study had some level of social support, as indicated by the presence of a confidant, our results indicate that those one in twenty migraineurs without a confidant may be particularly vulnerable to adverse mental health outcomes. It is also important to consider that some migraineurs may report having a confidant, but this does not necessarily mean they are actively engaging with them, particularly if their pain limits them from doing so. Further research is needed to determine ways that migraineurs can better access helpful social relationships to reduce social isolation and depression.
Consistent with previous studies examining the socioeconomic correlates of CMH in the general population, our study found that migraineurs in the highest household income bracket had significantly higher odds of CMH than those in the lowest household income bracket 16, 68. While the exact mechanism by which income influences mental health status among migraineurs is unclear, it may be partially explained by the role of socioeconomic status in determining quality of life among migraineurs. Individuals with higher incomes typically have greater access to resources for treating migraine symptoms 69, 70. In contrast, lower socioeconomic status is associated with several factors that increase disease prevalence and severity, including higher levels of stress, poor diet, and limited access to health care 71. These findings emphasize the importance of effective symptom management, particularly among migraineurs with lower incomes who may be less likely to access resources that can mitigate migraine symptom-related disability.
Study Strengths & Limitations
The present study has several limitations that should be acknowledged when considering our findings. First, migraine status was determined by self-reported health professional diagnosis in the CCHS-MH. While previous research shows that self-report of physician diagnosis correctly identifies migraineurs from a population-based sample approximately 75% of the time 72, it is still important to consider that less than half of migraineurs have received medical attention for their conditions, and only about a quarter have been diagnosed and report using an appropriate treatment 73. Given this finding, it is possible that many respondents who met the criteria for migraine were not captured by the survey because they did not have an official diagnosis, despite the fact that they may be suffering from this condition.
Second, the present study does not differentiate between specific migraine types such as migraine with or without aura, and episodic or chronic migraine. It is possible that the relationship between migraine and CMH may vary between different migraine types.
Third, because individuals residing in hospitals or other healthcare institutions were excluded from the CCHS-MH, individuals with very poor mental health are likely to be under-represented in the sample. Additionally, the CCHS-MH response rate was just under 70%, which raises concerns that there may be biases in the sample if individuals with more severe mental health issues and/or more severe migraine condition were less likely to participate. This could have skewed the sample towards those with higher levels of functioning, neglecting a particularly vulnerable subset of the population.
Finally, because this study utilized cross-sectional data, the direction of the associations between migraine, CMH, and various covariates could not always be determined. Consequently, the present study could not investigate whether some of the factors associated with CMH among migraineurs, such as insomnia and depression, were predictors or outcomes of migraine. Further, because this study used discrete, categorical data, we are limited in our ability to explore incremental relationships among certain variables, such as income and CMH, and instead examined the association between income categories and CMH.
The present study also has several notable strengths. First, this study used a large, nationally representative, population-based sample, which demonstrates its potential to be extrapolated to the broader population of migraineurs. Second, this study utilized the WHO-CIDI composite index, a validated instrument for assessing depression and anxiety status. Additionally, CMH was assessed using the Mental Health Continuum Short Form, a validated instrument with excellent internal consistency 12.
An additional strength of the present study is that it provides clinicians and health care providers with guidance on how to best support individuals suffering from migraine, and ultimately help them achieve CMH. By demonstrating that it is the underlying comorbidities, such as depression and chronic pain, that separate migraineurs from the general population in achieving CMH, this paper provides a clear point of intervention for healthcare professionals. This is a hopeful finding for individuals suffering from migraine that may feel as though CMH is out of their grasp, as this paper demonstrates the high potential for increased quality of life by addressing the comorbidities of migraine.
Conclusion
This study demonstrates that the inverse relationship between migraine and CMH appears to be explained by the mental and physical health comorbidities of migraine. Among those with migraine, strong correlates of CMH include a lack of history of depression, the presence of a confidant, and an income of $80,000 or more. The results of the present study may be used to tailor migraine interventions to optimize the odds of achieving CMH. In addition to treating symptoms of migraine, clinicians and health care providers should focus on addressing these co-occurring physical and mental health issues to support the overall well-being of migraineurs.
Acknowledgements
The authors would like to thank Andie MacNeil for her assistance with manuscript preparation and the Social Sciences and Humanities Research Council for funding this project.
Declarations/Disclosures
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Social Sciences and Humanities Research Council Grant [# 435-2016-0660].
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
- Buse DC, Silberstein SD, Manack AN, Papapetropoulos S, Lipton RB. Psychiatric comorbidities of episodic and chronic migraine. J Neurol. Aug 2013;260(8):1960-9. PubMed PMID: 23132299. doi:10.1007/s00415-012-6725-x
- Buse DC, Manack A, Serrano D, Turkel C, Lipton RB. Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J Neurol Neurosurg Psychiatry. Apr 2010;81(4):428-32. PubMed PMID: 20164501. doi:10.1136/jnnp.2009.192492
- Uhlig BL, Engstrom M, Odegard SS, Hagen KK, Sand T. Headache and insomnia in population-based epidemiological studies. Cephalalgia. Sep 2014;34(10):745-51. PubMed PMID: 24973418. doi:10.1177/0333102414540058
- Fuller-Thomson E, Schrumm M, Brennenstuhl S. Migraine and Despair: Factors Associated with Depression and Suicidal Ideation among Canadian Migraineurs in a Population-Based Study. Depress Res Treat. 2013;2013:401487. PubMed PMID: 24224086; PubMed Central PMCID: PMCPMC3810321. doi:10.1155/2013/401487
- Fuller-Thomson E, Jayanthikumar J, Agbeyaka SK. Untangling the Association Between Migraine, Pain, and Anxiety: Examining Migraine and Generalized Anxiety Disorders in a Canadian Population Based Study. Headache. Mar 2017;57(3):375-390. PubMed PMID: 27991658. doi:10.1111/head.13010
- Fuller-Thomson E, Hodgins GA. Suicide Attempts among Those with Migraine: Findings from a Nationally Representative Canadian Study. Arch Suicide Res. 2020;24(sup1):360-379. PubMed PMID: 30945611. doi:10.1080/13811118.2019.1578710
- Jette N, Patten S, Williams J, Becker W, Wiebe S. Comorbidity of migraine and psychiatric disorders–a national population-based study. Headache. Apr 2008;48(4):501-16. PubMed PMID: 18070059. doi:10.1111/j.1526-4610.2007.00993.x
- Ashina S, Serrano D, Lipton RB, et al. Depression and risk of transformation of episodic to chronic migraine. J Headache Pain. Nov 2012;13(8):615-24. PubMed PMID: 23007859; PubMed Central PMCID: PMCPMC3484253. doi:10.1007/s10194-012-0479-9
- Keyes CL, Simoes EJ. To flourish or not: positive mental health and all-cause mortality. Am J Public Health. Nov 2012;102(11):2164-72. PubMed PMID: 22994191; PubMed Central PMCID: PMCPMC3477942. doi:10.2105/AJPH.2012.300918
- Keyes CL. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am Psychol. Feb-Mar 2007;62(2):95-108. PubMed PMID: 17324035. doi:10.1037/0003-066X.62.2.95
- Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. Jun 2002;43(2):207-22. PubMed PMID: 12096700.
- Westerhof GJ, Keyes CL. Mental Illness and Mental Health: The Two Continua Model Across the Lifespan. J Adult Dev. Jun 2010;17(2):110-119. PubMed PMID: 20502508; PubMed Central PMCID: PMCPMC2866965. doi:10.1007/s10804-009-9082-y
- Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. Jul-Aug 2001;41(7):646-57. PubMed PMID: 11554952. doi:10.1046/j.1526-4610.2001.041007646.x
- Lyngberg AC, Rasmussen BK, Jorgensen T, Jensen R. Incidence of primary headache: a Danish epidemiologic follow-up study. Am J Epidemiol. Jun 1 2005;161(11):1066-73. PubMed PMID: 15901627. doi:10.1093/aje/kwi139
- Ramage-Morin PL, Gilmour H. Prevalence of migraine in the Canadian household population. Health Rep. Jun 2014;25(6):10-6. PubMed PMID: 24941316.
- Gilmour H. Positive mental health and mental illness. Health Rep. Sep 2014;25(9):3-9. PubMed PMID: 25229895.
- Bigal ME, Liberman JN, Lipton RB. Obesity and migraine: a population study. Neurology. Feb 28 2006;66(4):545-50. PubMed PMID: 16354886. doi:10.1212/01.wnl.0000197218.05284.82
- Bigal ME, Tsang A, Loder E, Serrano D, Reed ML, Lipton RB. Body mass index and episodic headaches: a population-based study. Arch Intern Med. Oct 8 2007;167(18):1964-70. PubMed PMID: 17923596. doi:10.1001/archinte.167.18.1964
- Schramm SH, Obermann M, Katsarava Z, Diener HC, Moebus S, Yoon MS. Epidemiological profiles of patients with chronic migraine and chronic tension-type headache. J Headache Pain. May 7 2013;14:40. PubMed PMID: 23651174; PubMed Central PMCID: PMCPMC3655106. doi:10.1186/1129-2377-14-40
- Bigal ME, Lipton RB. Excessive opioid use and the development of chronic migraine. Pain. Apr 2009;142(3):179-182. PubMed PMID: 19232469. doi:10.1016/j.pain.2009.01.013
- Stuginski-Barbosa J, Dach F, Bigal M, Speciali JG. Chronic pain and depression in the quality of life of women with migraine–a controlled study. Headache. Mar 2012;52(3):400-8. PubMed PMID: 22332812. doi:10.1111/j.1526-4610.2012.02095.x
- Raggi A, Giovannetti AM, Quintas R, et al. A systematic review of the psychosocial difficulties relevant to patients with migraine. J Headache Pain. Nov 2012;13(8):595-606. PubMed PMID: 23001069; PubMed Central PMCID: PMCPMC3484254. doi:10.1007/s10194-012-0482-1
- Molarius A, Tegelberg A, Ohrvik J. Socio-economic factors, lifestyle, and headache disorders – a population-based study in Sweden. Headache. Nov-Dec 2008;48(10):1426-37. PubMed PMID: 18624712. doi:10.1111/j.1526-4610.2008.01178.x
- Brennenstuhl S, Fuller-Thomson E. The Painful Legacy of Childhood Violence: Migraine Headaches Among Adult Survivors of Adverse Childhood Experiences. Headache. Jul-Aug 2015;55(7):973-83. PubMed PMID: 26104222. doi:10.1111/head.12614
- Tietjen GE, Brandes JL, Digre KB, et al. History of childhood maltreatment is associated with comorbid depression in women with migraine. Neurology. Sep 4 2007;69(10):959-68. PubMed PMID: 17785664. doi:10.1212/01.wnl.0000271383.60376.67
- Fuller-Thomson E, Brennenstuhl S, Frank J. The association between childhood physical abuse and heart disease in adulthood: findings from a representative community sample. Child Abuse Negl. Sep 2010;34(9):689-98. PubMed PMID: 20663556. doi:10.1016/j.chiabu.2010.02.005
- Tietjen GE, Herial NA, Hardgrove J, Utley C, White L. Migraine comorbidity constellations. Headache. Jun 2007;47(6):857-65. PubMed PMID: 17578536. doi:10.1111/j.1526-4610.2007.00814.x
- Fuller-Thomson E, Baker TM, Brennenstuhl S. Investigating the association between childhood physical abuse and migraine. Headache. May 2010;50(5):749-60. PubMed PMID: 20236339. doi:10.1111/j.1526-4610.2010.01626.x
- Centers for Disease C, Prevention. Adverse childhood experiences reported by adults — five states, 2009. MMWR Morb Mortal Wkly Rep. Dec 17 2010;59(49):1609-13. PubMed PMID: 21160456.
- Bell D, Belicki K. A community-based study of well-being in adults reporting childhood abuse. Child Abuse Negl. Jul 1998;22(7):681-5. PubMed PMID: 9693846. doi:10.1016/s0145-2134(98)00045-3
- Bellis MA, Lowey H, Leckenby N, Hughes K, Harrison D. Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. J Public Health (Oxf). Mar 2014;36(1):81-91. PubMed PMID: 23587573. doi:10.1093/pubmed/fdt038
- Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child Abuse Negl. Nov 2013;37(11):917-25. PubMed PMID: 23978575; PubMed Central PMCID: PMCPMC4090696. doi:10.1016/j.chiabu.2013.07.011
- Peres MF, Lucchetti G. Coping strategies in chronic pain. Curr Pain Headache Rep. Oct 2010;14(5):331-8. PubMed PMID: 20680705. doi:10.1007/s11916-010-0137-3
- Wachholtz AB, Pearce MJ. Does spirituality as a coping mechanism help or hinder coping with chronic pain? Curr Pain Headache Rep. Apr 2009;13(2):127-32. PubMed PMID: 19272278. doi:10.1007/s11916-009-0022-0
- Amin FM, Aristeidou S, Baraldi C, et al. The association between migraine and physical exercise. J Headache Pain. Sep 10 2018;19(1):83. PubMed PMID: 30203180; PubMed Central PMCID: PMCPMC6134860. doi:10.1186/s10194-018-0902-y
- Daenen L, Varkey E, Kellmann M, Nijs J. Exercise, not to exercise, or how to exercise in patients with chronic pain? Applying science to practice. Clin J Pain. Feb 2015;31(2):108-14. PubMed PMID: 24662498. doi:10.1097/AJP.0000000000000099
- Fuller-Thomson E, Lacombe-Duncan A. Understanding the Association Between Chronic Obstructive Pulmonary Disease and Current Anxiety: A Population-Based Study. COPD. Oct 2016;13(5):622-31. PubMed PMID: 26830204. doi:10.3109/15412555.2015.1132691
- Fuller-Thomson E, Roane JL, Brennenstuhl S. Three Types of Adverse Childhood Experiences, and Alcohol and Drug Dependence Among Adults: An Investigation Using Population-Based Data. Subst Use Misuse. Sep 18 2016;51(11):1451-61. PubMed PMID: 27326749. doi:10.1080/10826084.2016.1181089
- Fuller-Thomson E, West KJ. Flourishing despite a cancer diagnosis: factors associated with complete mental health in a nationally-representative sample of cancer patients aged 50 years and older. Aging Ment Health. Sep 2019;23(9):1263-1274. PubMed PMID: 30130417. doi:10.1080/13607863.2018.1481926
- Fuller-Thomson E, West KJ, Sulman J, Baird SL. Childhood Maltreatment Is Associated with Ulcerative Colitis but Not Crohn’s Disease: Findings from a Population-based Study. Inflamm Bowel Dis. Nov 2015;21(11):2640-8. PubMed PMID: 26230860. doi:10.1097/MIB.0000000000000551
- Fuller-Thomson E, Lateef R, Sulman J. Robust Association Between Inflammatory Bowel Disease and Generalized Anxiety Disorder: Findings from a Nationally Representative Canadian Study. Inflamm Bowel Dis. Oct 2015;21(10):2341-8. PubMed PMID: 26218145. doi:10.1097/MIB.0000000000000518
- Fuller-Thomson E, Ramzan N, Baird SL. Arthritis and suicide attempts: findings from a large nationally representative Canadian survey. Rheumatol Int. Sep 2016;36(9):1237-48. PubMed PMID: 27306384. doi:10.1007/s00296-016-3498-z
- Statistics Canada. Canadian Community Health Survey – Mental Health (CCHS). Accessed May 27, 2021, https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5015
- Lamers SM, Westerhof GJ, Bohlmeijer ET, ten Klooster PM, Keyes CL. Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF). J Clin Psychol. Jan 2011;67(1):99-110. PubMed PMID: 20973032. doi:10.1002/jclp.20741
- Statistics Canada. (2013) Canadian community health Survey–Mental health (CCHS) Derived Variable (DV) Specifications. Ottawa, Canada: Statistics Canada.
- Wittchen HU. Reliability and validity studies of the WHO–Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. Jan-Feb 1994;28(1):57-84. PubMed PMID: 8064641. doi:10.1016/0022-3956(94)90036-1
- Hamelsky SW, Lipton RB. Psychiatric comorbidity of migraine. Headache. Oct 2006;46(9):1327-33. PubMed PMID: 17040330. doi:10.1111/j.1526-4610.2006.00576.x
- Ligthart L, Gerrits MM, Boomsma DI, Penninx BW. Anxiety and depression are associated with migraine and pain in general: an investigation of the interrelationships. J Pain. Apr 2013;14(4):363-70. PubMed PMID: 23395476. doi:10.1016/j.jpain.2012.12.006
- Ligthart L, Nyholt DR, Penninx BW, Boomsma DI. The shared genetics of migraine and anxious depression. Headache. Nov 2010;50(10):1549-60. PubMed PMID: 20553331. doi:10.1111/j.1526-4610.2010.01705.x
- Finocchi C, Villani V, Casucci G. Therapeutic strategies in migraine patients with mood and anxiety disorders: clinical evidence. Neurol Sci. Jun 2010;31 Suppl 1:S95-8. PubMed PMID: 20464594. doi:10.1007/s10072-010-0297-2
- Baskin SM, Smitherman TA. Comorbidity between migraine and depression: update on traditional and alternative treatments. Neurol Sci. May 2011;32 Suppl 1:S9-13. PubMed PMID: 21533704. doi:10.1007/s10072-011-0549-9
- Kang EH, Park JE, Chung CS, Yu BH. Effect of biofeedback-assisted autogenic training on headache activity and mood states in Korean female migraine patients. J Korean Med Sci. Oct 2009;24(5):936-40. PubMed PMID: 19794995; PubMed Central PMCID: PMCPMC2752780. doi:10.3346/jkms.2009.24.5.936
- Vasudeva S, Claggett AL, Tietjen GE, McGrady AV. Biofeedback-assisted relaxation in migraine headache: relationship to cerebral blood flow velocity in the middle cerebral artery. Headache. Mar 2003;43(3):245-50. PubMed PMID: 12603643. doi:10.1046/j.1526-4610.2003.03048.x
- Gardner A, Boles RG. Beyond the serotonin hypothesis: mitochondria, inflammation and neurodegeneration in major depression and affective spectrum disorders. Prog Neuropsychopharmacol Biol Psychiatry. Apr 29 2011;35(3):730-43. PubMed PMID: 20691744. doi:10.1016/j.pnpbp.2010.07.030
- Carod-Artal FJ. Tackling chronic migraine: current perspectives. J Pain Res. 2014;7:185-94. PubMed PMID: 24748814; PubMed Central PMCID: PMCPMC3986300. doi:10.2147/JPR.S61819
- Ong JC, Park M. Chronic headaches and insomnia: working toward a biobehavioral model. Cephalalgia. Oct 2012;32(14):1059-70. PubMed PMID: 22875878. doi:10.1177/0333102412455709
- Fox KR. The influence of physical activity on mental well-being. Public Health Nutr. Sep 1999;2(3A):411-8. PubMed PMID: 10610081. doi:10.1017/s1368980099000567
- Grant N, Wardle J, Steptoe A. The relationship between life satisfaction and health behavior: a cross-cultural analysis of young adults. Int J Behav Med. 2009;16(3):259-68. PubMed PMID: 19319695. doi:10.1007/s12529-009-9032-x
- Goodwin R. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;2003 Jun(36(6)):698-703. PubMed Central PMCID: PMC12744913. doi:10.1016/s0091-7435(03)00042-2
- Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. Jun 2003;36(6):698-703. PubMed PMID: 12744913. doi:10.1016/s0091-7435(03)00042-2
- Headache Classification Committee of the International Headache S. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. Jul 2013;33(9):629-808. PubMed PMID: 23771276. doi:10.1177/0333102413485658
- Fuller-Thomson E, Agbeyaka S, LaFond DM, Bern-Klug M. Flourishing after depression: Factors associated with achieving complete mental health among those with a history of depression. Psychiatry Res. Aug 30 2016;242:111-120. PubMed PMID: 27267442. doi:10.1016/j.psychres.2016.04.041
- Fuller-Thomson E, Ryckman K. Achieving complete mental health despite a history of generalized anxiety disorders: Findings from a large, nationally representative Canadian survey. J Affect Disord. Mar 15 2020;265:687-694. PubMed PMID: 32090786. doi:10.1016/j.jad.2019.12.004
- Baiden P, Fuller-Thomson E. Factors Associated with Achieving Complete Mental Health among Individuals with Lifetime Suicidal Ideation. Suicide Life Threat Behav. Aug 2016;46(4):427-46. PubMed PMID: 26811142. doi:10.1111/sltb.12230
- Fuller-Thomson E, Jensen LA. Flourishing After a Stroke: A Nationally Representative Portrait of Resilience and Mental Health Among Older Canadians. J Aging Health. Jun/Jul 2020;32(5-6):308-316. PubMed PMID: 30624141. doi:10.1177/0898264318822228
- Manack AN, Buse DC, Lipton RB. Chronic migraine: epidemiology and disease burden. Curr Pain Headache Rep. Feb 2011;15(1):70-8. PubMed PMID: 21063918. doi:10.1007/s11916-010-0157-z
- Helvig AW, Minick P. Adolescents and headaches: maintaining control. Pediatr Nurs. Jan-Feb 2013;39(1):19-25; quiz 26. PubMed PMID: 23540101.
- Stewart WF, Roy J, Lipton RB. Migraine prevalence, socioeconomic status, and social causation. Neurology. Sep 10 2013;81(11):948-55. PubMed PMID: 23990405; PubMed Central PMCID: PMCPMC3888198. doi:10.1212/WNL.0b013e3182a43b32
- Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA. Jan 1 1992;267(1):64-9. PubMed PMID: 1727198.
- Lipton RB, Serrano D, Holland S, Fanning KM, Reed ML, Buse DC. Barriers to the diagnosis and treatment of migraine: effects of sex, income, and headache features. Headache. Jan 2013;53(1):81-92. PubMed PMID: 23078241. doi:10.1111/j.1526-4610.2012.02265.x
- Bigal ME, Lipton RB, Winner P, et al. Migraine in adolescents: association with socioeconomic status and family history. Neurology. Jul 3 2007;69(1):16-25. PubMed PMID: 17606878. doi:10.1212/01.wnl.0000265212.90735.64
- Warren JW, Clauw DJ. Functional somatic syndromes: sensitivities and specificities of self-reports of physician diagnosis. Psychosom Med. Nov-Dec 2012;74(9):891-5. PubMed PMID: 23071343. doi:10.1097/PSY.0b013e31827264aa
- Lipton RB, Scher AI, Kolodner K, Liberman J, Steiner TJ, Stewart WF. Migraine in the United States: epidemiology and patterns of health care use. Neurology. Mar 26 2002;58(6):885-94. PubMed PMID: 11914403. doi:10.1212/wnl.58.6.885
Acknowledgements
The authors would like to thank Andie MacNeil for her assistance with manuscript preparation and the Social Sciences and Humanities Research Council for funding this project.
Declarations/Disclosures
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Social Sciences and Humanities Research Council Grant [# 435-2016-0660].
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
