Author: G Niraj* MD 1, Peter Critchley MD 2
Author Affiliation:
1 Consultant in Pain Medicine, Clinical Research Unit in Pain Medicine, University Hospitals of Leicester NHS Trust
2 Consultant in Neurology, Clinical Research Unit in Pain Medicine, University Hospitals of Leicester NHS Trust
Competing Interests: The author/s declare no competing interests.
Issue: 08.01
DOI: 10.30756/ahmj.2022.08.01
Received: Aug 29, 2022
Revised: Nov 13, 2022
Accepted: Nov 15, 2022
Published: Dec 16, 2022
Recommended Citation: Niraj G, Critchley P. Intermediate Cervical Plexus Block (ICPB) In Refractory Chronic Daily Headache After Whiplash: Prospective Audit In 43 Patients. Ann Head Med. 2022;08:01. DOI: 10.30756/ahmj.2022.08.01
Background: Chronic daily headache can develop or pre-existing episodic headache can worsen after whiplash and is termed persistent headache attributed to whiplash. It can be a therapeutic challenge and often results in severe disability. The objective was to assess the management of patients with refractory secondary chronic daily headache referred to a pain physician in consideration for greater occipital nerve block.
Methods: Prospective service evaluation in adult patients with oro-facial pain and headaches. Patients underwent specialist neurology review and analgesic overuse headache was excluded. Patients with chronic daily headache with a past history of neck trauma were included. Cervical facet joint dysfunction and intracranial pathology were excluded. An initial cohort of 27 patients received occipital nerve block without benefit. Subsequently, all patients were offered ultrasound guided intermediate cervical plexus block with local anesthetic and steroid mixture. Four-week headache diary, Brief Pain Inventory-Short Form and Hospital Anxiety Depression Scale questionnaires were completed at baseline and three months post-intervention.
Results: Over a 41-month period, 43 patients were reviewed. The first 27 patients (27/43, 63%) reported no benefit with occipital nerve block. Subsequently, patients were offered intermediate cervical plexus block(s). Four patients refused. Thirty-nine patients received the intervention. Thirty-two patients (32/39, 82%) reported significant reduction in headache frequency and intensity at three months. Failure rate was 18% (7/39).
Conclusion: The cervical plexus could play a significant role in the development or worsening of pre-existing headache after whiplash. Intermediate cervical plexus block may have a role in the management of refractory chronic daily headache following whiplash injury.
Introduction
Chronic daily headache (CDH) implies headache on a daily or near daily basis, that can be a therapeutic challenge and often results in significant morbidity 1. It is classified into primary and secondary CDH 1. Secondary CDH following neck trauma or whiplash is classified as persistent headache attributed to whiplash 2. Management strategies includes abortive and prophylactic agents, greater occipital nerve block and Botulinum toxin-A (non-licensed use)2, 3. In patients who fail to respond, treatment options are limited.
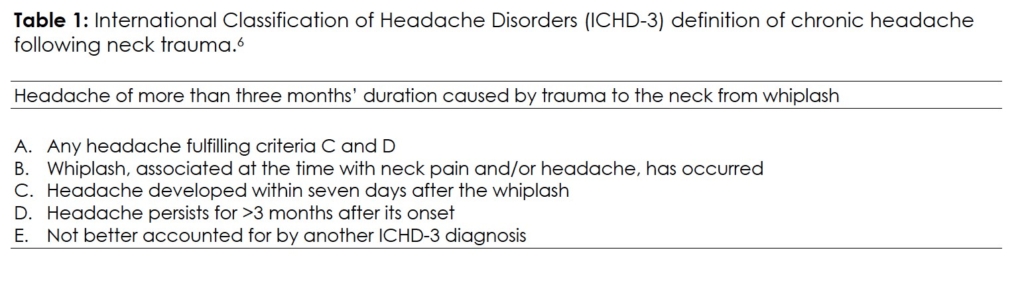
Whiplash-associated disorder (WAD) includes an array of symptoms that follows sudden acceleration-deceleration trauma to the head and neck 4. Headache is a common presentation that can persist beyond three months in over a third of cases 5. The International Classification of Headache Disorders (ICHD-3) has defined the diagnostic criteria for persistent headache following whiplash trauma to the neck (Table 1) 6. Cervical zygapophyseal joint dysfunction is the recognized pathology in a subset of patients with whiplash with a gold standard treatment, namely cervical medial branch thermal radiofrequency neurotomy 7, 8. Recently, alternate pain generators identified include the cervicothoracic muscles and upper cervical nerves 9-11. In addition, the trigemino-cervical complex, which includes the cervical plexus, appears to play a key role in the pathogenesis of chronic headaches following whiplash 12, 13. The authors present the first report on ultrasound-guided intermediate cervical plexus block with steroid in the management of refractory persistent headache attributed to whiplash.
Methods
The prospective audit was performed at a tertiary pain medicine unit at a University Teaching hospital and was registered with the Clinical Audit Safety and Effectiveness registry (CASE 8161) 14. Patients were referred by the neurology team in consideration for greater occipital nerve block(s) between 2018 and 2021. The referring physician excluded analgesic overuse headache. Informed written consent was obtained for their de-identified data to be used for analysis and for publication.
Patients meeting the International Classification of Headache Disorders (ICHD-3) diagnostic criteria for persistent headache from whiplash were included (Table 1) 6. Criterion C was not strictly adhered in patient selection1. The presenting complaint was chronic daily headache, and all patients reported a history of neck trauma preceding the development of CDH. The time frame (range) between the trauma and the onset of persistent headache is detailed in Table 2. Secondary CDH in this report was defined as headache occurring at least 15 days per month as a result of neck trauma 1, 2.
All patients underwent diagnostic magnetic resonance imaging (MRI) of the head to rule out intracranial pathology. A specialist neurologist ruled out medication overuse headache. Cervical zygapophyseal joint dysfunction was excluded in the pain clinic (limitation of extension at cervical spine, pain on cervical zygapophyseal joint loading manoeuvres, tenderness on palpation over cervical zygapophyseal joints and MRI of cervical spine, if indicated) 15.
In our series, refractory CDH was defined as failure to respond to standard management including prophylactic and abortive medications and greater occipital nerve block(s) and or Botulinum toxin A. The number of prophylactic and abortive medications trialed is detailed in (Table 2). We have included Botulinum toxin A in this criterion since a subset of patients who presented with migraine-like headaches received Botulinum toxin A prior to pain clinic referral. Patients with refractory CDH were offered ICPB.
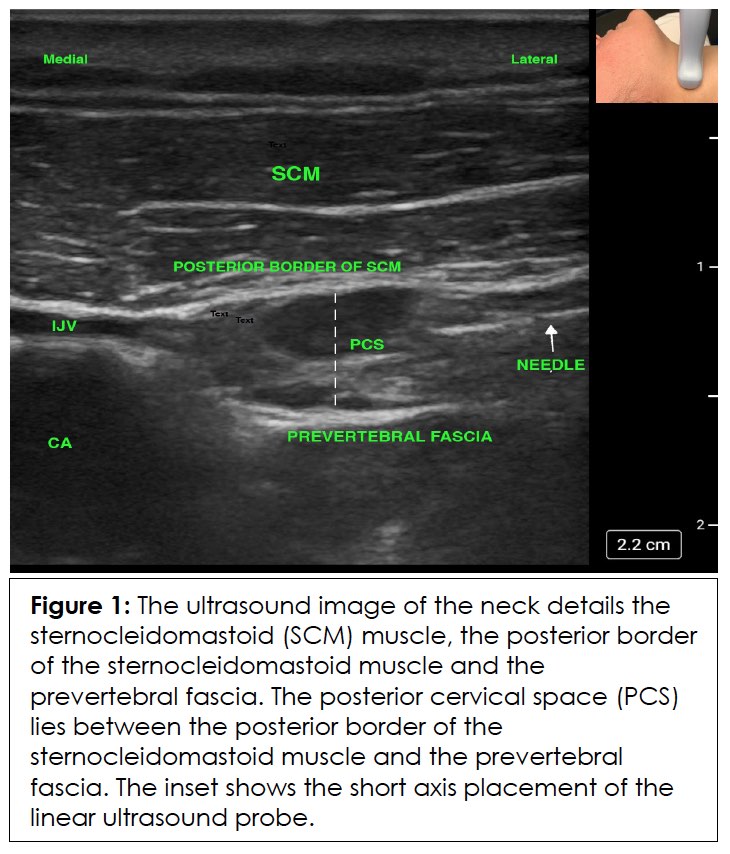
Ultrasound guided intermediate cervical plexus block 16
The procedure was performed under local anesthesia in the outpatient suite. The patient was positioned in the lateral decubitus position. The skin over the sternocleidomastoid muscle was prepared with 2% chlorhexidine solution. A high frequency (5-10 MHz) ultrasound probe (S-NerveTM; SonoSite Inc., Washington, USA) was placed across the sternocleidomastoid muscle at the third cervical vertebral level. The muscle, the underlying vascular structures and the posterior cervical space (PCS, fascial plane between the posterior sheath of the muscle and the prevertebral fascia, Figure 1) were visualized. Thereafter, a 23-gauge 50 mm hypodermic needle was inserted in the plane of the ultrasound beam towards the posterior cervical space (Figure 1). Once the needle entered the PCS, 9 ml of a mixture of 1% lidocaine and depot methylprednisolone (60 mg) was injected after negative aspiration. The procedure was repeated on the contralateral side, if the patient complained of bilateral headache.
Pre-ICPB, patients completed a headache diary for four weeks, Brief Pain Inventory short form (BPI-SF) and Hospital Anxiety and Depression scale (HADS) questionnaires. Post ICPB, patients completed a four week headache diary in the third month in addition to BPI-SF and HADS questionnaires.
Data collected included age, gender, duration of CDH, past history of headaches, employment status, incidence of phrenic nerve palsy after ICPB (postprocedural dyspnoea), Horner’s syndrome and post-procedural flare-up of headache.
In the audit, clinically significant pain relief was defined using the ‘Pain at its worst in the last 24 hours’ construct in the Brief Pain Inventory Short Form (BPI SF) questionnaire. This 11-point pain intensity Numerical Rating Scale (NRS) has been found to have the strongest relationship with the pain interference scale 17. Following IMMPACT recommendations (Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials), a 2-point change (30-36%) at three months post treatment was considered as successful intervention 18. A 4-point change (>50) at 3-month post treatment was considered as durable treatment 19.
Statistical analysis was performed using Stata version 13.1 (Statacorp LC, Texas) statistical package for Windows (Microsoft Corp.). The paired t test was used to compare the changes in the frequency of headache days, BPI score and HADS score at baseline and at three months. Differences were considered significant for P < 0.05. Missing data was imputed using the ‘last-observation-carried-forward’ method.
Results
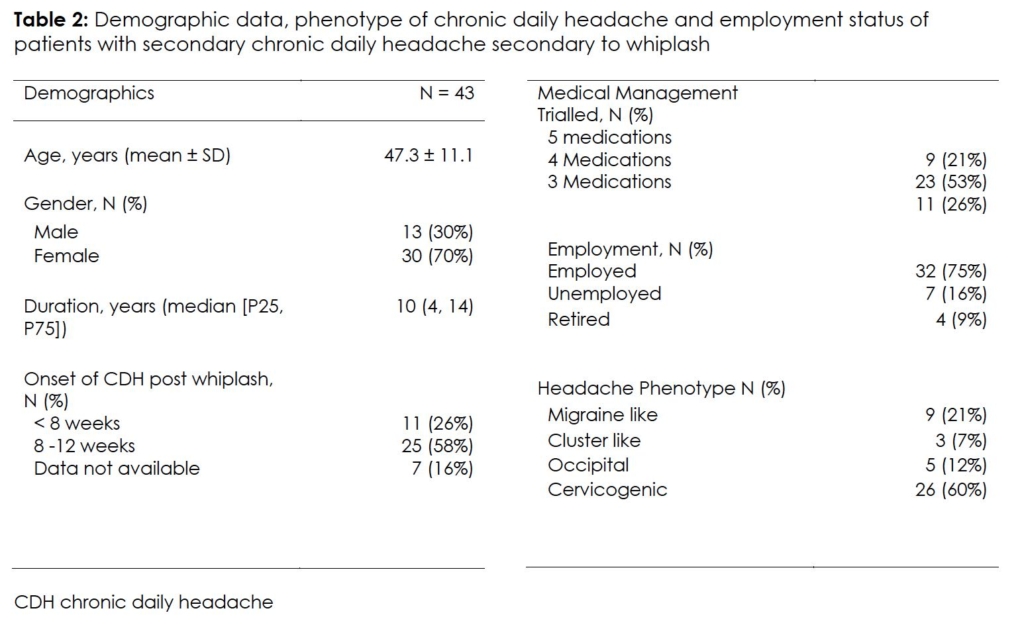
Over a 41-month period, 43 patients were referred to the pain clinic with refractory CDH. All patients reported a history of neck trauma prior to the onset of headaches or worsening of pre-existing episodic headache (Table 2). A past history of headache before the onset of trauma was present in 11 patients (11/43, 26%). The phenotype included migraine (8/11, 73%) and tension type headache (3/11, 27%).
Prior to pain clinic referral, 11 patients (11/43, 26%) received Botulinum toxin A (as per PREEMPT protocol) and reported no benefit. Under the pain physician, the first 27 patients (27/43, 63%) received ultrasound guided greater occipital nerve block(s) with depot steroid and reported transient (< 4 weeks) or no benefit. Subsequently, all 43 patients were offered intermediate cervical plexus block(s) with depot steroid. Four patients (4/43, 9%) refused both interventions (occipital nerve block and ICPB) due to needle phobia.
Intermediate cervical plexus block was performed in 39 patients. Bilateral ICPB was performed in 24 patients (24/39, 62%) who reported bilateral symptoms. Demographic details and patient characteristics are provided in Table 2. Cervical zygapophyseal joint dysfunction was excluded in all patients.
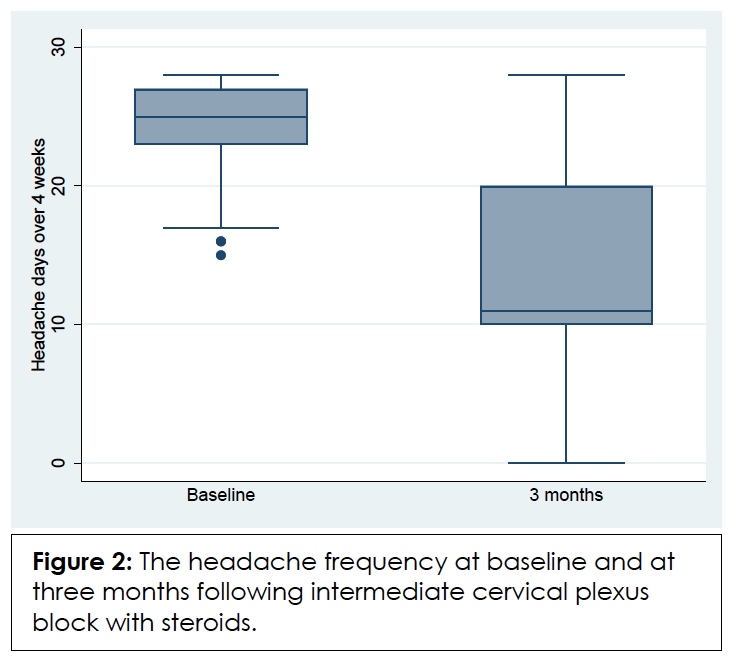
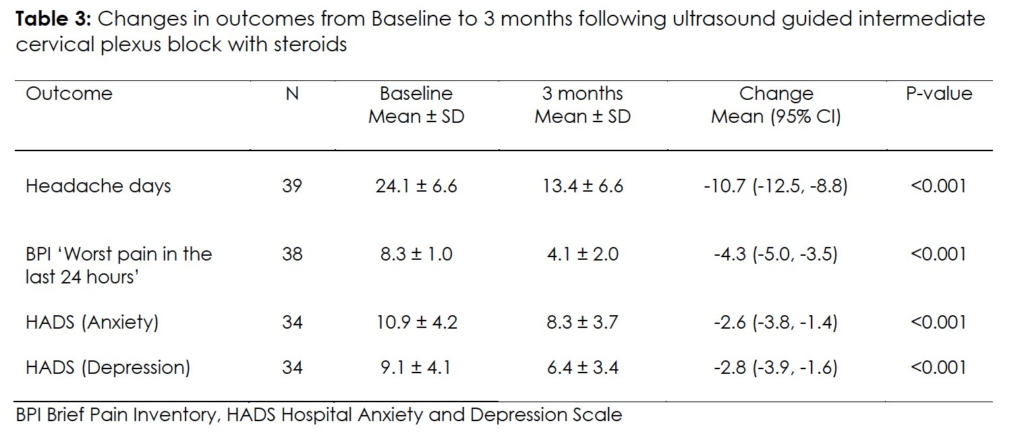
Following ICPB, clinically significant relief was observed in 32 patients (32/39, 82%). Patients reported onset of relief within 3-10 days post-ICPB. Twenty-five patients (25/39, 64%) reported durable relief (>50% reduction at three-month follow-up). Seven patients (7/39, 18%) failed to report any benefit (Figure 2). There was significant improvement in pain and mood at three-month follow-up (Table 3).
Thirty patients were struggling to maintain employment due to severity of CDH and were considering either reducing hours or leaving work. Post ICPB, 27 patients (27/30, 90%) who responded to ICPB were able to maintain employment.
Twenty-three patients (23/39, 59%) reported post-procedural flare-up for 1- 2 weeks. There were no instances of dyspnoea secondary to phrenic nerve palsy despite 62% of patients receiving bilateral ICPB. None of the patients developed overt signs of cervical sympathetic block (Horner’s syndrome). Missing data was imputed in seven patients.
Tables
Discussion
Intermediate cervical plexus block provided significant reduction in headache frequency and intensity at three months in 82% patients (32/39) with refractory CDH and a history of whiplash. In addition, there was improvement in mood that enabled patients to maintain employment. A past history of headaches, considered a risk factor for persistent headache after whiplash, was present in 11 patients (11/43, 26%). Seven patients (7/39, 18%) failed to respond to ICPB.
Headaches are the second commonest presentation after neck pain and can persist at 12 months in 38% following whiplash 5. The ICHD (beta 3) has defined the diagnostic criteria for persistent headache after whiplash 6. However, this definition includes a strict criterion ‘C’ that limits the definition to those patients who have developed headache within seven days of whiplash. In this series, we included patients with a history of trauma to the neck prior to onset of CDH or worsening of pre-existing episodic headaches. Non-adherence to criterion C enabled a larger pool of patients with secondary CDH post neck trauma to receive ICPB.
A well-established pain generator in a subset of patients with whiplash is the cervical zygapophyseal joint dysfunction 7. None of the patients showed clinical signs of cervical zygapophyseal joint dysfunction. Recent evidence suggests alternate pain generators including the cervicothoracic musculature and upper cervical nerves 9-11. During flexion-hyperextension trauma to the neck, there is significant stress on the cervicothoracic muscles 10. This traumatic impact can affect the cervical plexus as they are closely related to these muscles11. Thus, persistent headache following neck trauma could involve a nociceptive drive from the upper cervical afferents as a result of rotational injury 20. In addition, there is evidence of neurophysiologic and structural convergence of cervical sensory and muscle afferent inputs onto the trigeminal subnucleus caudalis neurons 12-14, 21-23. This fits in with one of the proposed mechanisms for the pathogenesis of headache following neck trauma namely, trigeminal sensory system activation 13.
During ICPB, the injectate is deposited in the posterior cervical space above the prevertebral fascia (Figure 1) 24. There is robust evidence that demonstrates the permeation of injected solution through the porous prevertebral fascia thereby blocking the deep cervical plexus 24-28. In addition, the sympathetic chain could be exposed to the injectate 16. Although, none of our patients had overt signs of sympathetic block (Horner’s syndrome), the possibility of suppression of sympathetic activity cannot be ruled out. Thus, a single ultrasound-guided injection can target multiple cervical neural pathways thereby downregulating the sensitized trigemino-cervical complex. This may explain the benefit of ICPB in neck pain, headache and facial pain following head and neck trauma 11, 16, 24.
Standard management strategies were unsuccessful in our cohort. A subset of patients failed to respond to Botulinum Toxin A (11/43, 26%) or greater occipital nerve block (27/43, 63%), which target the muscles and nerves of the scalp. Thus, the failure of these interventions as well as significant analgesia observed with ICPB supports the hypothesis that the cervical plexus could be a dominant pain generator in whiplash. Ultrasound-guided ICPB has an excellent safety profile and can be performed in the outpatient clinic 11, 16.
The authors are aware of the limitations to the open label case series in a small group of patients under a single physician. Non-adherence to the criterion C of the IHS definition of persistent headache post-whiplash allowed a larger cohort to receive IICPB. Refractory secondary CDH can cause severe disability. Any intervention with a good safety profile that can be performed at an outpatient setting and provides durable relief mandates evaluation. There is potential concern on the use of depot steroid in the neck region. However, performing the intervention under real time ultrasound guidance as well as negative aspiration prior to injecting the mixture reduces the risk of inadvertent intravascular injection. In addition, the mixture is injected in a fascial plane (posterior cervical space).
Conclusion
In conclusion, the cervical plexus could play an important role in persistence of symptoms after whiplash. Intermediate cervical plexus block with steroid may have a role in the management of refractory secondary CDH following neck trauma. Definitive studies are required to confirm this observation.
References
- Couch JR. Update on chronic daily headache. Curr Treat Options Neurol. Feb 2011;13(1):41-55. PubMed PMID: 21103961. doi:10.1007/s11940-010-0104-7
- Halker RB, Hastriter EV, Dodick DW. Chronic daily headache: an evidence-based and systematic approach to a challenging problem. Neurology. Feb 15 2011;76(7 Suppl 2):S37-43. PubMed PMID: 21321350. doi:10.1212/WNL.0b013e31820d5f32
- Gupta R, Fisher K, Pyati S. Chronic Headache: a Review of Interventional Treatment Strategies in Headache Management. Curr Pain Headache Rep. Jul 29 2019;23(9):1-9. PubMed PMID: 31359257. doi:10.1007/s11916-019-0806-9
- Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine (Phila Pa 1976). Apr 15 1995;20(8 Suppl):1S-73S. PubMed PMID: 7604354.
- Al-Khazali HM, Ashina H, Iljazi A, et al. Neck pain and headache after whiplash injury: a systematic review and meta-analysis. Pain. May 2020;161(5):880-888. PubMed PMID: 31977938. doi:10.1097/j.pain.0000000000001805
- Headache Classification Committee of the International Headache S. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. Jul 2013;33(9):629-808. PubMed PMID: 23771276. doi:10.1177/0333102413485658
- Lord SM, Barnsley L, Wallis BJ, Bogduk N. Chronic cervical zygapophysial joint pain after whiplash. A placebo-controlled prevalence study. Spine (Phila Pa 1976). Aug 1 1996;21(15):1737-44; discussion 1744-5. PubMed PMID: 8855458. doi:10.1097/00007632-199608010-00005
- Engel A, Rappard G, King W, Kennedy DJ, Standards Division of the International Spine Intervention S. The Effectiveness and Risks of Fluoroscopically-Guided Cervical Medial Branch Thermal Radiofrequency Neurotomy: A Systematic Review with Comprehensive Analysis of the Published Data. Pain Med. Apr 2016;17(4):658-69. PubMed PMID: 26359589. doi:10.1111/pme.12928
- Heneghan NR, Smith R, Rushton A. Thoracic dysfunction in whiplash-associated disorders: a systematic review and meta-analysis protocol. Syst Rev. Feb 9 2016;5:26. PubMed PMID: 26860082; PubMed Central PMCID: PMCPMC4748634. doi:10.1186/s13643-016-0201-0
- Vasavada AN, Brault JR, Siegmund GP. Musculotendon and fascicle strains in anterior and posterior neck muscles during whiplash injury. Spine (Phila Pa 1976). Apr 1 2007;32(7):756-65. PubMed PMID: 17414909. doi:10.1097/01.brs.0000259058.00460.69
- James A, Niraj G. Intermediate Cervical Plexus Block: A Novel Intervention in the Management of Refractory Chronic Neck and Upper Back Pain Following Whiplash Injury: A Case Report. A A Pract. Apr 2020;14(6):e01197. PubMed PMID: 32784315. doi:10.1213/XAA.0000000000001197
- Watson DH, Drummond PD. The Role of the Trigemino Cervical Complex in Chronic Whiplash Associated Headache: A Cross Sectional Study. Headache. Jun 2016;56(6):961-75. PubMed PMID: 27091393. doi:10.1111/head.12805
- Ashina H, Porreca F, Anderson T, et al. Post-traumatic headache: epidemiology and pathophysiological insights. Nat Rev Neurol. Oct 2019;15(10):607-617. PubMed PMID: 31527806. doi:10.1038/s41582-019-0243-8
- Niraj G, Simpson L, Raithatha B. Interventional Management of Refractory Trigeminal Neuropathic Pain: A Prospective Audit of a Novel Management Pathway in 70 Patients. Pain Physician. Sep 2020;23(5):E525-E534. PubMed PMID: 32967403.
- McCormick ZL, Walega DR. Cervical epidural steroid injection for refractory somatic tinnitus. Pain Pract. Feb 2015;15(2):e28-33. PubMed PMID: 25353360. doi:10.1111/papr.12255
- Lee H, Simpson L, Niraj G. Intermediate Cervical Plexus Block for Refractory Bilateral Facial Pain From a Whiplash Injury in 3 Patients: A Case Report. A A Pract. Aug 1 2022;16(8):e01612. PubMed PMID: 35952333. doi:10.1213/XAA.0000000000001612
- Atkinson TM, Mendoza TR, Sit L, et al. The Brief Pain Inventory and its “pain at its worst in the last 24 hours” item: clinical trial endpoint considerations. Pain Med. Mar 2010;11(3):337-46. PubMed PMID: 20030743; PubMed Central PMCID: PMCPMC3806650. doi:10.1111/j.1526-4637.2009.00774.x
- Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. Feb 2008;9(2):105-21. PubMed PMID: 18055266. doi:10.1016/j.jpain.2007.09.005
- Niraj G. Pathophysiology and Management of Abdominal Myofascial Pain Syndrome (AMPS): A Three-Year Prospective Audit of a Management Pathway in 120 Patients. Pain Med. Nov 1 2018;19(11):2256-2266. PubMed PMID: 29444277. doi:10.1093/pm/pnx343
- Packard RC. The relationship of neck injury and post-traumatic headache. Curr Pain Headache Rep. Aug 2002;6(4):301-7. PubMed PMID: 12095465. doi:10.1007/s11916-002-0051-4
- Piovesan EJ, Kowacs PA, Oshinsky ML. Convergence of cervical and trigeminal sensory afferents. Curr Pain Headache Rep. Oct 2003;7(5):377-83. PubMed PMID: 12946291. doi:10.1007/s11916-003-0037-x
- Browne PA, Clark GT, Kuboki T, Adachi NY. Concurrent cervical and craniofacial pain. A review of empiric and basic science evidence. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. Dec 1998;86(6):633-40. PubMed PMID: 9868716. doi:10.1016/s1079-2104(98)90195-0
- Sessle BJ, Hu JW, Amano N, Zhong G. Convergence of cutaneous, tooth pulp, visceral, neck and muscle afferents onto nociceptive and non-nociceptive neurones in trigeminal subnucleus caudalis (medullary dorsal horn) and its implications for referred pain. Pain. Nov 1986;27(2):219-235. PubMed PMID: 3797017. doi:10.1016/0304-3959(86)90213-7
- Niraj G. Intermediate cervical plexus block in the management of treatment resistant chronic cluster headache following whiplash trauma in three patients: a case series. Scand J Pain. Aug 18 2022;PubMed PMID: 35977523. doi:10.1515/sjpain-2022-0058
- Pandit JJ, Satya-Krishna R, Gration P. Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth. Aug 2007;99(2):159-69. PubMed PMID: 17576970. doi:10.1093/bja/aem160
- Opperer M, Kaufmann R, Meissnitzer M, et al. Depth of cervical plexus block and phrenic nerve blockade: a randomized trial. Reg Anesth Pain Med. Apr 2022;47(4):205-211. PubMed PMID: 35012992; PubMed Central PMCID: PMCPMC8867263. doi:10.1136/rapm-2021-102851
- Nash L, Nicholson HD, Zhang M. Does the investing layer of the deep cervical fascia exist? Anesthesiology. Nov 2005;103(5):962-8. PubMed PMID: 16249670. doi:10.1097/00000542-200511000-00010
- Kim HY, Soh EY, Lee J, et al. Incidence of hemi-diaphragmatic paresis after ultrasound-guided intermediate cervical plexus block: a prospective observational study. J Anesth. Aug 2020;34(4):483-490. PubMed PMID: 32236682. doi:10.1007/s00540-020-02770-2
Acknowledgement
The author would like to sincerely thank the chronic pain specialist nursing team at University Hospitals of NHS Trust, Leicester for performing the post-procedural follow-up of patients.
Declarations/Disclosures
Consent/Permissions: Audit Registration: CASE 8161
Funding: University Hospitals of Leicester NHS Trust supported the project
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, author declares the following:
Payment/services info: Author has declared that no financial support was received from any organization for the submitted work.
Financial relationships: Author have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: Author have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
