Author: Leon S. Moskatel * MD 1, Nathaniel M. Schuster MD 2
Author Affiliation:
1 Department of Neurology, Division of Headache, Stanford Health Care, Palo Alto, CA, USA
2 Pain and Headache Neurologist, Center for Pain Medicine, Department of Anesthesiology, University of California, San Diego, La Jolla, CA, USA
Competing Interests: The author/s declare no competing interests.
Issue: 06.03
DOI: 10.30756/ahmj.2021.06.03
Received: Nov 16, 2021
Revised: Dec 29, 2021
Accepted: Dec 30, 2021
Published: Jan 13, 2022
Recommended Citation: Moskatel LS, Schuster NM. Medication-Overuse Headache: Results from a Pain Medicine Clinic Cohort. Ann Head Med. 2021;06:03. DOI: 10.30756/ahmj.2021.06.03
Background and Objective: Medication-overuse headache (MOH) is a common, disabling, and treatable cause of chronic daily headache. This study evaluates the characteristics of a cohort of patients with MOH seen in a pain medicine clinic.
Methods: We conducted a retrospective study of consecutive patients seen by a neurologist in the pain medicine clinic at the University of California, San Diego. Demographics, headache diagnoses, and overused medications were extracted from clinical records from 83 patients ≥ 18 years of age where a diagnosis of MOH was entered into the electronic medical record September 12, 2017-March 30, 2020.
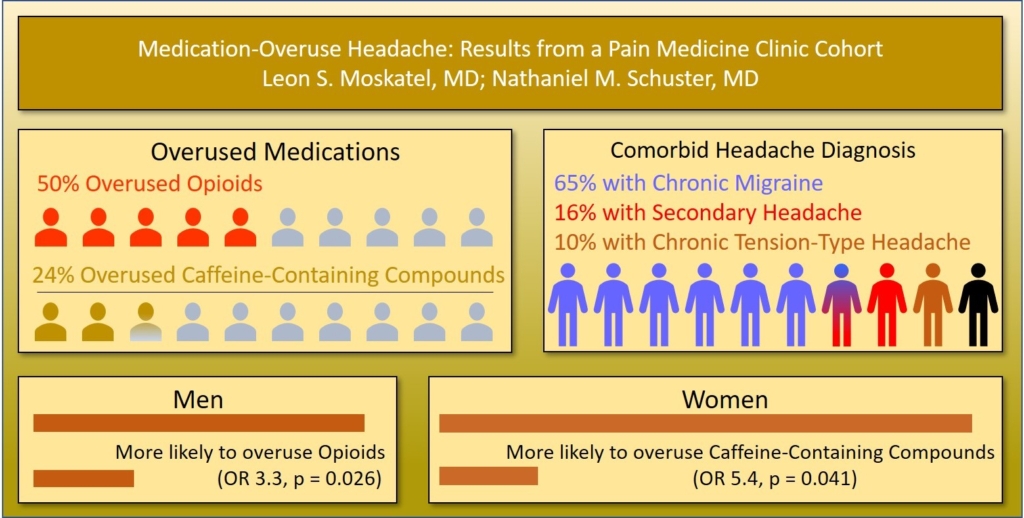
Results: Opioids were the most overused medications (42/83, 50.6%) followed by caffeine-containing compounds (20/83, 24.1%), triptans (12/83, 14.5%) and non-steroidal anti-inflammatory drugs (10/83, 12.9%). Chronic migraine was the most common underlying headache syndrome (54/83, 65.1%), followed by secondary headache disorder (13/83, 15.7%) and tension-type headache (8/83, 9.6%). Men were more likely to be overusing opioids (OR 3.3, p = 0.026) while women were more likely to be overusing caffeine-containing compounds (OR 5.4, p = 0.041).
Discussion and Conclusions: It is crucial for pain specialists to recognize MOH in the pain clinic setting. Opioid overuse headache is more common among men, likely in part due to migraine being underrecognized in men and therefore men not receiving migraine-specific medications. Caffeine-containing compound overuse is more common among women; these are over-the-counter (OTC) and often do not appear on patients’ medications lists. Pain specialists should specifically ask patients with headache whether they are using OTC caffeine-containing compounds.
Introduction
Medication-overuse headache (MOH) frequently presents as a comorbid condition in the therapeutic course of primary headache disorders. It is defined by the International Classification of Headache Disorders Third edition (ICHD-3) as a headache occurring on at least 15 days per month in a patient with a pre-existing headache disorder, use >15 days per month of acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) or >10 days per month of ergots, triptans, opioids, or combination analgesics for at least 3 months of one or more drugs that can be taken for acute and/or symptomatic treatment of headache, and is not better accounted for by another ICHD-3 diagnosis (ICHD-3) 1. This secondary headache affects 60 million individuals worldwide and is among the top 20 causes of disability worldwide 2. Prevalence varies between 0.5% to 7.2% depending on the group assessed and has been found to be 4 times as common in women than men 3, 4. In pain clinics, MOH has been found to be as prevalent as 29% of patients with chronic pain 5. Numerous risk factors have been associated with the development of medication-overuse headache including obesity, anxiety or depression, physical inactivity, low educational level, smoking, and age less than 50 6-9.
Despite initial attribution of MOH solely to ergotamines, the phenomenon now includes most acute medications that can be applied for the treatment of headache including simple and combination analgesics, triptans, opioids, and barbiturates 10. Studies conducted in different countries and over different years have found different acute medications being most commonly overused. However, previously, ergotamines have been the most frequently used medication leading to MOH 11. Conversely, in a 2004 study of 4855 patients older than 14 years in Spain, acetaminophen was most commonly overused (54%) followed in turn by caffeine (49%) and ergotamine (38%) 12. Notably, this occurred in relative proximity to the rollout of the triptan class of medications, and the 3% of patients overusing triptans and 38% of patients overusing ergotamine is reflective of that time in history. This is critical as triptans and ergotamines have been found to be more likely to induce MOH than analgesics 13. However, pain clinics likely see a population of headache patients different from those seen in primary care or neurology clinics given referral patterns of patients on opioids often to chronic pain clinics.
Limited evidence suggests that pain practitioners are less likely to diagnosis medication overuse headache than are neurologists. In a different recent study conducted at the UCSD Center for Pain Medicine, among a cohort of patients receiving occipital nerve blocks, 6.5% of patients who had been evaluated by a neurologist had been diagnosed with medication overuse headache, while 0 patients exclusively under the treatment of a pain anesthesiologist or pain physiatrist had been diagnosed with medication overuse headache 14. Our study seeks to expand the literature as the first study to identify what classes of medications are most frequently overused by patients with MOH seeking treatment in a pain clinic.
Materials and Methods
This retrospective study (UCSD IRB #200543) included consecutive patients seen by a single neurologist (NMS) boarded in both headache medicine and pain medicine for a new patient visit between September 12, 2017, and March 30, 2020, for which the diagnosis of medication overuse headache was entered into the electronic medical records, yielding a cohort of 83 patients, drawing from referrals from primary care providers, neurologists, and other pain physicians. The medications overused were those documented at the time of the new patient visit and prescription medications (including opioids) had been prescribed by providers outside the pain clinic for headache and/or non-cephalic pain. Continuous outcomes were described by means and standard deviations. Categorical outcomes were described by percentages and odds ratios. Diagnoses were made according to the ICHD-3 with the exception that patients with secondary headache disorders were diagnosed with medication overuse headache when suspected by the treating clinician, despite the ICHD-3 stating that medication-overuse headache occurs in “Patients with a pre-existing primary headache.” This is reflective of the clinician’s practice to recommend a trial of tapering off overused analgesics in patients with secondary headache disorders with headaches occurring >15 days per month.
Results
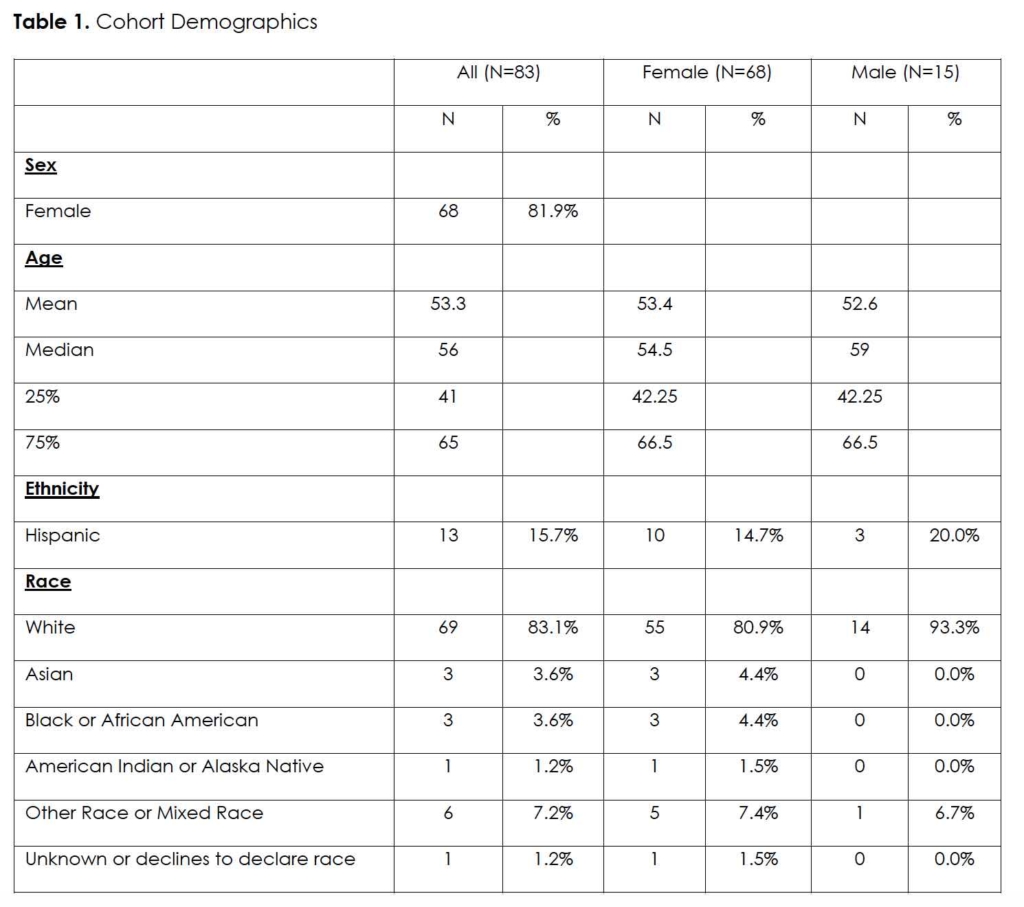
Out of the 83 patients, 68 (81.9%) were female with a mean age of 53.3. 69 (83.1%) patients were white, 6 (7.2%) other race, 3 (3.6%) of both Asian or African-American, and 1(1.2%) each of American Indian or unknown. 13 (15.7%) were Hispanic (Table 1).
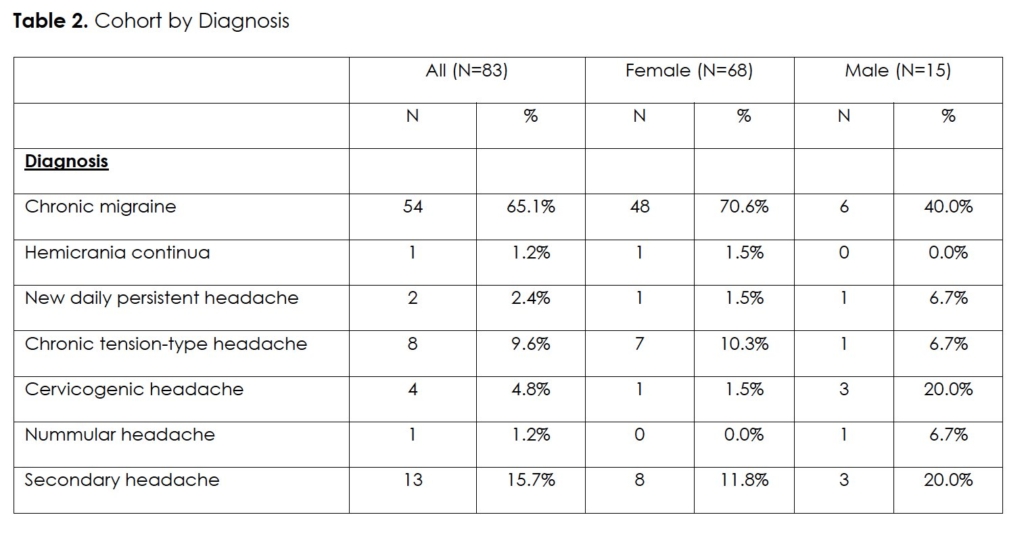
By definition, patients with medication overuse headache have an additional headache diagnosis. 54 (65.1%) of our patients carried a diagnosis of chronic migraine. The next most common diagnosis was that of a different secondary headache disorder in 13 (15.7%). Chronic tension-type headache contributed 8 (9.6%) of cases. The rest of the cases included 4 (4.8%) with cervicogenic headache, 2 (2.4%) with new daily persistent headache, and 1 (1.2%) each of hemicrania continua and nummular headache (Table 2).
In terms of the medications overused (Table 3), opioids were overused in 42 (50.6%) of patients. 17 (39.5%) of these patients overused oxycodone, with hydrocodone being the second most common overused opioid with 12 (27.9) of these patients overusing it.
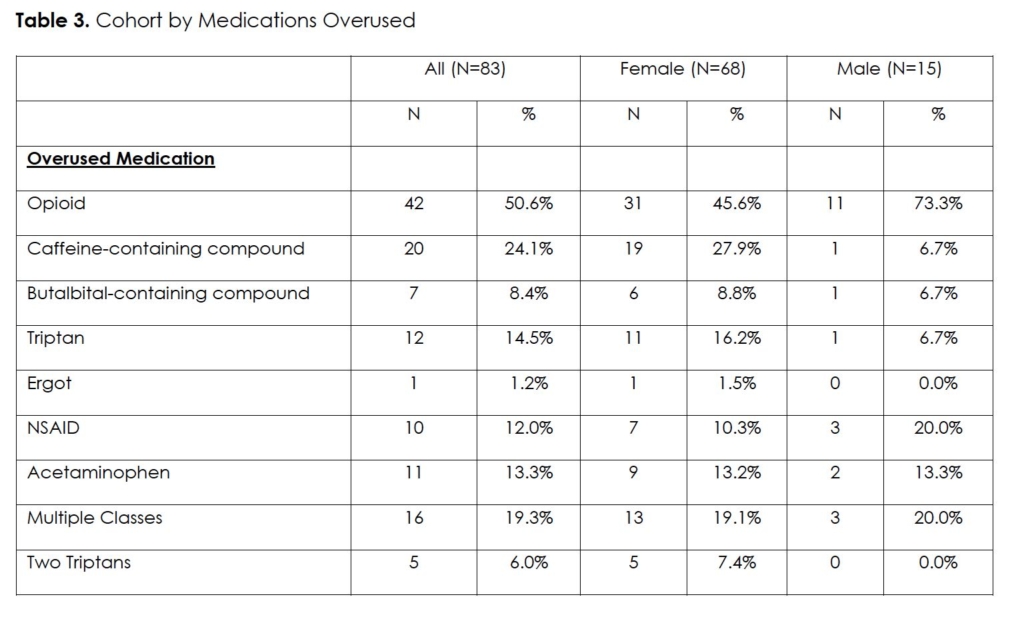
Caffeine-containing compounds were also overused with 20 (24.1%) patients. Triptans and NSAIDs had similar rates of overuse with triptans at 12 (14.5%) patients and NSAIDs with 10 (12.0%) patients. Sumatriptan was the most overused triptan, accounting for half of the triptans used, 10 (50%) of the 20 triptans used across 12 patients.
Acetaminophen (excluding combination analgesics containing acetaminophen) was overused in 11 (13.3%) of patients. Acetaminophen-containing compounds were overused by 45 (54.2%) of patients using either acetaminophen alone or in a combination formulation such as acetaminophen-caffeine-aspirin in 19 patients (42.2%) of this acetaminophen-using cohort or oxycodone-acetaminophen in 8 patients (17.8%) and hydrocodone-acetaminophen in 7 patients (15.6%).
Multiple medications from different classes were overused in 16 (19.3%) of patients. NSAIDs were most frequently used in combination with other medications in 11 (13.3%) followed by acetaminophen in 8 (9.6%) of patients, triptans in 7 (8.4%) of patients, and opioids in 6 (7.2%) patients. Butalbital-containing compounds and caffeine-containing compounds were rarely used in conjunction with other medications with only 2 (2.4%) patients and 1 (1.2%) patient, respectively.
When the medications prompting overuse are compared by sex, men were more likely to overuse opioids (OR 3.3, p = 0.026) while women were more likely to overuse caffeine-containing compounds (OR 5.4, p = 0.041). There was no statistical difference between men and women, reported here in OR for women, for butalbital-containing compounds (OR 1.4, p = 0.39), triptans (OR 2.7, p = 0.17), NSAIDs (OR 0.5, p = 0.38), acetaminophen (OR 0.9, p = 0.43), and multiple classes (OR 0.9, p = 0.47). An odds ratio could not be computed for ergots and dual triptan-use since no men in this sample were overusing those, however this difference was nonetheless not statistically significant (p = 0.14).
When considered by diagnosis, overuse of NSAIDs was more likely in both chronic migraine (OR 5.88, p = 0.013) and secondary headache (OR 7.2, p = 0.046) relative to chronic tension-type headache. Overuse of all other medication types in chronic migraine and secondary headache relative to chronic tension-type headache were not statistically significant.
Discussion
By definition, patients with medication overuse headache present with a separate primary headache diagnosis. Chronic migraine being the most diagnosed condition is unsurprising given that not only do intractable headaches make up a substantial cohort of a pain clinic, but medication overuse can also play a strong role in chronification from episodic to chronic migraine 15. Indeed, these patients are also often undertreated with preventative medications, leading to an increased reliance on rescue medications that can lead to MOH. Secondary headaches, excluding medication overuse headache, were the second most common situation in which MOH was diagnosed, a diagnosis made by the treating headache neurologist despite the ICHD-3 criteria for medication overuse headache specifying “in a patient with a pre-existing primary headache” when he recommended to the patient a trial of weaning off of frequently-used analgesic medications, with 69% (9/13) of patients with secondary headache disorders in this cohort being treated with opioids. A recent editorial published by Ashina and Dodick noted that the ICHD-3 are internally inconsistent with regards to whether patients with secondary headache disorders can be diagnosed with MOH 16. This study adds to the limited evidence about MOH in secondary headache disorders and supports revising MOH criteria to include patients with secondary headache disorders. This study also supports the need for more research into the treatment of patients with secondary headache disorders, and especially for non-opioid treatments. Future research should study the response of patients with secondary headache disorders to slowly weaning off of opioids and other frequently used analgesics to demonstrate whether medication overuse headache can occur in patients with secondary headache disorders. If so, this may warrant removing the clause of “in a patient with a pre-existing primary headache” from the definition of MOH in future iterations of the ICHD.
A population survey has shown that nationally, 15.3% of patients overusing medications use opioids 17. Our pain clinic cohort had a more than three times higher rate of opioid overuse. This high rate of opioid use in our cohort demonstrates a likely concentration of patients with opioid-overuse headache being referred to pain clinics rather than to headache or neurology clinics, as well as referral of patients with opioid-overuse headaches from headache and neurology clinics to pain clinics. Patients using opioids for headaches have also been shown to have a higher number of headache days per month relative to opioid nonusers as well as more use of simple analgesics 17. Since such patients are often treated in pain clinics, it is important for providers in pain clinics to be educated about medication overuse headache recognition and treatment. For example, pain physicians should know that the diagnosis of opioid-overuse headache can be made in the presence of “Regular intake of one or more opioids on ≥10 days/month for >3 months” and is believed to be associated with the number of days per month that opioids are used rather than the number of milligram morphine equivalents used per day 1, 15. Caffeine-overuse, in the form predominantly of acetaminophen-aspirin-caffeine formulations, is also unsurprising given the strong direct-to-consumer marketing of these medications and their perceived effectiveness. The high prevalence of use of acetaminophen is due to its frequent incorporation in combination formulations such as opioid-acetaminophen, butalbital-acetaminophen-caffeine, and acetaminophen-aspirin-caffeine. This data set is unable to discern to what extent the acetaminophen in these formulations contributes to the development of MOH.
Regarding sex-based risk for specific medications for overuse, among the myriad medications assessed, only increased male risk for opioid overuse and female risk for caffeine-containing compounds were statistically significant. This could potentially stem from known provider minimization of female pain resulting in a higher use of over-the-counter medications such as acetaminophen-caffeine-aspirin, while more frequent prescribing of opioids in male patients with migraine has been reported in other studies and may be a result of migraine diagnosis being missed and guidelines-recommended migraine treatments such as triptans being less likely to be used in male patients as well as male patients not having their complaints minimized and receiving opioids by well-intentioned but misguided providers 18.
When assessed by disease, patients with chronic tension-type headache were more likely to overuse NSAIDs relative to chronic migraine and secondary headache. This may be due to the paucity of evidence-based effective treatments for chronic tension-type headache resulting in these patients often self-treating with over-the-counter medication. No other medications were more prevalent in chronic tension-type headache relative to chronic migraine and secondary headache.
Fortunately, only 8.4% of patients in this cohort of patients with medication overuse headache were overusing butalbital-containing compounds, reflecting likely reduced prescribing patterns of this class of medications in the studied community. Butalbital-containing compounds have been known to convey a high risk of medication overuse headache and can result in dependence and a dangerous withdrawal syndrome, leading to them being removed from the market in many countries, but they continue to be marketed in the US. Their routine use has been discouraged by medical societies including the American Headache Society Choosing Wisely campaign 19. Similarly, ergotamines were only overused by a single patient in the study, likely reflecting the decreased routine use of this older class of medication with the expanding pharmacopeia of headache management.
Limitations of this study include sample size of 83 consecutive patients and that it is reflective of a single pain center practice and a single provider. The limited number of non-white patients and male patients is similar to that of many headache studies. With only 16.9% of patients being non-white there was limited ability to dissect what role race and ethnicity played in the overuse of specific medications. Similarly, with only 15 (18.9%) male patients, the study was not sufficiently powered to detect many differences in specific medications and conditions that could give providers additional guidance in the treatment of this population. While of adequate sample size to assess relative rates of use of overused medications in patients with chronic migraine, the comparatively few cases of other forms of chronic headaches comorbid with medication overuse headache precluded further analysis. While this study is believed to be the first of its kind to describe relative rates of overused medications in an American pain clinic, medication prescribing patterns might be different in other geographical locations within the US as well as in other countries. This study did not follow patient outcomes for response to discontinuation of overused medications.
Future work to describe patterns of medication overuse headache in pain clinics should include larger studies involving additional pain clinics. Future studies should also include interventions to increase the recognition of medication overuse headache among pain physicians and long-term outcomes of weaning and discontinuation of opioids (and other overused medications) in patients with secondary headache disorders with headaches occurring >15 days per month. If patients with secondary headache disorders benefit from weaning of overused acute medications, future iterations of the ICHD-3 should redefine medication-overuse headache to include patients with secondary headache disorders.
Conclusion
Pain practitioners should be aware of the diagnosis of medication overuse headache, particularly in opioid users, as its recognition and treatment can help patients with chronic headache disorders transform back to having episodic headaches. Our study adds to the literature an analysis of an American cohort of patients with MOH in a pain clinic. We found a more than three times higher rate of overuse of opioids than that found in a large survey of the US population with MOH and also found high rates of overuse of caffeine-containing compounds. In addition, we have showed that, similar to in a survey of the overall US population, male sex is also a risk factor for opioid overuse in the pain clinic setting, and that female sex is a risk factor for caffeine-containing compound overuse. Reducing MOH in the long run will be achieved through better education of first contact providers for patients, continuing to address the opioid epidemic, and through counseling patients on appropriate use of over-the-counter medications such as NSAIDs, acetaminophen, and caffeine-containing compounds.
References
- H G. 8.2 Medication-overuse headache (MOH). ICHD-3. . Accessed April 27, 2021, 2021. https://ichd-3.org/8-headache-attributed-to-a-substance-or-its-withdrawal/8-2-medication-overuse-headache-moh/
- Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. Oct 8 2016;388(10053):1545-1602. PubMed PMID: 27733282; PubMed Central PMCID: PMCPMC5055577. doi:10.1016/S0140-6736(16)31678-6
- Westergaard ML, Hansen EH, Glumer C, Olesen J, Jensen RH. Definitions of medication-overuse headache in population-based studies and their implications on prevalence estimates: a systematic review. Cephalalgia. May 2014;34(6):409-25. PubMed PMID: 24293089. doi:10.1177/0333102413512033
- Westergaard ML, Glumer C, Hansen EH, Jensen RH. Medication overuse, healthy lifestyle behaviour and stress in chronic headache: Results from a population-based representative survey. Cephalalgia. Jan 2016;36(1):15-28. PubMed PMID: 25804645. doi:10.1177/0333102415578430
- Schmid CW, Maurer K, Schmid DM, et al. Prevalence of medication overuse headache in an interdisciplinary pain clinic. J Headache Pain. Jan 30 2013;14:4. PubMed PMID: 23565761; PubMed Central PMCID: PMCPMC3606964. doi:10.1186/1129-2377-14-4
- He Z, Dong L, Zhang Y, Kong Q, Tan G, Zhou J. Metabolic syndrome in female migraine patients is associated with medication overuse headache: a clinic-based study in China. Eur J Neurol. Aug 2015;22(8):1228-34. PubMed PMID: 25981360. doi:10.1111/ene.12732
- Hagen K, Linde M, Steiner TJ, Stovner LJ, Zwart JA. Risk factors for medication-overuse headache: an 11-year follow-up study. The Nord-Trondelag Health Studies. Pain. Jan 2012;153(1):56-61. PubMed PMID: 22018971. doi:10.1016/j.pain.2011.08.018
- Westergaard ML, Glumer C, Hansen EH, Jensen RH. Prevalence of chronic headache with and without medication overuse: associations with socioeconomic position and physical and mental health status. Pain. Oct 2014;155(10):2005-13. PubMed PMID: 25020001. doi:10.1016/j.pain.2014.07.002
- Schwedt TJ, Alam A, Reed ML, et al. Factors associated with acute medication overuse in people with migraine: results from the 2017 migraine in America symptoms and treatment (MAST) study. J Headache Pain. May 24 2018;19(1):38. PubMed PMID: 29797100; PubMed Central PMCID: PMCPMC5968010. doi:10.1186/s10194-018-0865-z
- Evers S, Marziniak M. Clinical features, pathophysiology, and treatment of medication-overuse headache. Lancet Neurol. Apr 2010;9(4):391-401. PubMed PMID: 20298963. doi:10.1016/S1474-4422(10)70008-9
- Ravishankar K. Medication overuse headache in India. Cephalalgia. Nov 2008;28(11):1223-6. PubMed PMID: 18983591. doi:10.1111/j.1468-2982.2008.01731.x
- Gupta VK. Chronic daily headache with analgesic overuse: epidemiology and impact on quality of life. Neurology. Oct 12 2004;63(7):1341; author reply 1341. PubMed PMID: 15477578. doi:10.1212/wnl.63.7.1341
- Ferrari A, Leone S, Vergoni AV, et al. Similarities and differences between chronic migraine and episodic migraine. Headache. Jan 2007;47(1):65-72. PubMed PMID: 17355496. doi:10.1111/j.1526-4610.2006.00629.x
- Love S MC, Hopkins B, Schuster NM. Rates of migraine assessment, diagnosis, and treatment of patients receiving occipital nerve blocks in an academic pain clinic. 2021:
- Bigal ME, Serrano D, Buse D, Scher A, Stewart WF, Lipton RB. Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. Headache. Sep 2008;48(8):1157-68. PubMed PMID: 18808500. doi:10.1111/j.1526-4610.2008.01217.x
- Ashina H, Dodick DW. Medication-overuse headache in patients with secondary headache disorders: Need for revision? Headache. May 2021;61(5):790-791. PubMed PMID: 34105159. doi:10.1111/head.14108
- Lipton RB, Buse DC, Friedman BW, et al. Characterizing opioid use in a US population with migraine: Results from the CaMEO study. Neurology. Aug 4 2020;95(5):e457-e468. PubMed PMID: 32527971; PubMed Central PMCID: PMCPMC7455347. doi:10.1212/WNL.0000000000009324
- Schafer G, Prkachin KM, Kaseweter KA, Williams AC. Health care providers’ judgments in chronic pain: the influence of gender and trustworthiness. Pain. Aug 2016;157(8):1618-25. PubMed PMID: 26934512. doi:10.1097/j.pain.0000000000000536
- Choosing Wisely; Five Things Physicians and Patients Should Question. American Headache Society. Accessed June 28, 2021, 2021. https://www.choosingwisely.org/wp-content/uploads/2015/02/AHS-Choosing-Wisely-List.pdf
Declarations/Disclosures
Funding: None.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Financial relationships: LSM reports no conflicts of interest or disclosures. NMS is a section editor for Pain Medicine and the Annals of Headache Medicine, receives research support from the Migraine Research Foundation, and has received personal and/or consulting fees from Eli Lilly & Co., Lundbeck, and UMEHEAL.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
