Author: Pearl Angeli B. Diamante MD* 1, Artemio A. Roxas Jr. MD, FPNA 1,2
Author Affiliation:
1 Institute of Neurological Sciences, Department of Neurology, The Medical City, Philippines
2 University of the Philippines College of Medicine, Department of Neurosciences, Philippine General Hospital, Philippines
Competing Interests: The author/s declare no competing interests.
Issue: 04.01
DOI: 10.30756/ahmj.2020.04.01
Received: Sept 9, 2020
Revised: Oct 15, 2020
Accepted: Oct 16, 2020
Published: Oct 26, 2020
Recommended Citation: Diamante PAB, Roxas Jr AA. Music Medicine as a Component of Acute Migraine Attack Management in The Emergency Room: A Randomized Controlled Open-Label Trial. Ann Head Med. 2020;04:01. DOI: 10.30756/ahmj.2020.04.01
Background: Acute severe migraine requiring Emergency Room (ER) visit is managed by giving analgesics for pain relief. Since music medicine has been beneficial in other pain syndromes, the study of its effect as a noninvasive add-on to current management is worth pursuing.
Objective: To identify if music medicine in addition to medical therapy will reduce the severity and duration of an acute attack of moderate to severe migraine compared to medical management alone.
Methods: An open label randomized controlled trial was conducted at the ER of a tertiary hospital in the Philippines from July 2017 to June 2018. Patients who presented at the ER with acute moderate to severe headache fulfilling the ICH-3 criteria for migraine were included. They were randomized to medical therapy or to medical therapy with music medicine. A decrease in the severity of the headache after one hour of medical treatment was the primary outcome.
Results: One hundred eighty-three adult migraneurs were included without difference between group in age, gender, and occupation. There was a statistically significant reduction (p=0.037) in pain severity after one hour in 82 of 87 patients given medical treatment with music medicine (94%) compared to 73 of 86 in the medical therapy alone (85%). There were more headache-free patients at one hour in the music group (55% versus 42%, p=0.05).
Conclusion: There is decreased duration and severity of pain when music medicine is added to conventional medical therapy in treating patients with an acute migraine. This is the first randomized trial done in the acute ER setting.
Introduction
Background
Acute migraine headache is a common neurologic problem worldwide that reduces the quality of life of the affected individual 1. They are at times a source of emergency room (ER) admission, due to a persistent severe intensity and/or prolonged duration of an attack.
At the ER level, initial management of acute migraine consists of the use of analgesics to provide pain relief. Advances in the treatment of migraine such as the development of triptans has changed the lives of countless migraine patients but are not commonly used locally due to financial constraints. Thus, it is worth exploring a more cost-effective addition to medical management such as music medicine (MuMed), which has already been noted in other pain syndromes (e.g. cancer pain and procedural pain) 2, 3, 4, 5.
As of the year 2014, there are only four studies that investigated the effectiveness of MuMed in migraine; all of which utilized MuMed in chronic setting 6. At present, there are no studies that utilizes MuMed in an acute setting such as at the ER. This warrants investigation, more importantly in the Philippines because Filipinos are music-lovers by heart and the effect of music could be more pronounced. This is supported by a report from Spotify, one of the leading music-streaming platforms in the world at present, which stated that Filipinos spend on average 172 minutes per day listening to music. This makes the Philippines one of the biggest markets in Asia for the music-streaming platform 7.
Objectives
This study would like to determine if MuMed in addition to standard ER management will have a beneficial effect in the treatment of an acute migraine attack compared to medical management alone. Specifically, the investigators wanted to determine the effect of music in decreasing the severity of headache using a numeric pain rating scale in a span of 1 hour; as well as to determine the effect of MuMed in the duration of the attack. They also wanted to identify if MuMed has an effect in headache severity when measured at 30 minutes and 2 hours from initiation of the medical therapy.
Methods
Trial design
The study was an investigator-initiated, open-label randomized clinical trial conducted among adult patients who came in at the ER of a Joint Commission International (JCI) -accredited tertiary hospital. The hospital has a 20-bed ER capacity that is being supervised 24 hours daily by board certified ER consultants. It also has an accredited Emergency Medicine residency training program.
This study underwent full-board panel for ethical and technical review and was approved by the Institutional Review Board (IRB) of the hospital. Data was collected between July 2017 to June 2018 and informed consent was obtained from the patients prior to randomization. Patients did not receive any form of compensation for the participation in this study.
Participants
Migraineurs aged 18-60 years, who consulted at the E.R. with a complaint of an acute moderate to severe migraine attack with a numeric pain rating scale of 6-10/10 at 15 minutes post medication were included in the study. Migraineurs were identified based on the third edition of the International Classification of Headache Disorders. Patients were excluded if they (a) have an allergy to NSAIDS; (b) did not consent for the procedure; (c) have hearing impairments; (d) have a decreased sensorium; and (e) came to the ER alone, with no person accompanying them.
Sample size
The website www.powerandsamplesize.com was used to estimate the sample size. Studies on acute migraine relief noted that 48.3% of patients had improvement in their headache when given standard medical management as compared to placebo 8. The investigators assumed that there would be a 15% increase in relief with the addition of MuMed to the usual care, so they set the number to be 63% if MuMed was added. A total of 169 patients (85 per arm) was required to achieve a power of 80% and significance level= 0.05.
Randomization
Sequence generation
The website https://www.randomizer.org/ was used to generate random numbers in sets of 8. A blocked randomization was implemented to ensure equal distribution of the 2 arms. Half of the eight were numbered “1” which indicated treatment with medical therapy alone and the other half were numbered “2” for medical therapy with MuMed.
Allocation concealment mechanism
A total of 200 sealed envelopes were prepared and arranged in sequence, with each envelope containing a sheet of paper stating the intervention group the participant was to be randomized.
Implementation
After a participant has signed the consent form, the investigator took the first envelope to identify the patient’s intervention group. The indicated treatment arm written on the paper was then followed. This was done for all participants in order.
Interventions
The study protocol was discussed among all Neurology residents and each one of them were trained to administer the procedure when the primary investigator was unavailable.
The ER physician and residents were fully aware of the protocol. Patients seeking admission at the ER due to headache were seen by the ER physician. They were instructed to identify the baseline pain level of the patient by showing a numeric pain rating scale and asking them to point to the corresponding pain score they are currently feeling. After assessment of the ER physician and upon diagnosis of migraine attack with pain scale greater than or equal to 6, investigators were notified for potential participants. The ER physicians were allowed to choose their preferred medication, request laboratory and procedures as needed, secure referrals from specialized departments, and give additional medications as warranted. The investigators did not interfere with the management of the ER physicians.
The ER nurses then gave the pain medication as indicated in the doctor’s order, either through intravenous or oral route. Fifteen minutes after the medication was given, the ER physician reassessed the patient’s pain score. If the pain remained to be more than or equal to 6 over 10, the investigator or neurology resident will assess the participant. Once they confirmed the participant fulfilled the criteria for migraine, they were invited to the study. A lapse time of fifteen minutes was given to allow the patient to settle down and be provided with the appropriate care for their complaint prior to securing consent for involvement in the study.
Once the informed consent form was explained and signed, patients were then assigned in one of two arms of the study. Those who were randomized to the group receiving music medicine were given a standard in-ear earphones (Miniso brand) and an MP3 player (Tsinghua Tongfang brand). They were provided a list of genres to choose from and were instructed to pick one that they consider having a calming effect for them. Choices of genre included classical, pop, rock, jazz, R&B, meditation, religious, and Original Pilipino Music (OPM); and the playlists contained top 20-50 songs that were based on what was provided in Spotify, an internet-based music library. The participants were requested to choose only from the playlists and to use the equipment that the investigators provided. To ensure proper hygiene, earbuds were disposed after use of each participant and was replaced by a new one for each of the succeeding users. Music was placed on randomized mode and was played for at least 30 minutes. This was based on the most frequently used duration of music administration amongst the MuMed studies reviewed by Lee, et.al 9. Depending on the patient’s desire, it may be continued until the study is over. They were also allowed to adjust the volume of the music to their preference.
On the other hand, the control group was not given any device and they received only the medications ordered by the ER physician. For both groups, the investigator briefly asked for the severity of the patient’s headache after 30 minutes, 1 hour, and 2 hours (if the participant is still at the ER) from receiving the medication. No other additional interventions were provided such as massage, migraine counseling, or meditation.
If by any chance the participant noted discomfort and wished to withdraw from the study, they were allowed to do so at any point in the study. If there were allergic reactions noted secondary to the earphones used or if there were any other problems encountered during the duration of the study, the participant or the person accompanying them were instructed to notify the ER staff at once so they can in turn inform the investigators. Appropriate remedy was then provided.
To avoid other sources of confounding variables, lights were remained “on” for all the participants and were not placed in a special isolated room devoid of noise.
Outcomes
Participants were asked to rate the level of pain intensity on a 0-10 numeric pain rating scale. The primary outcome was an improvement of headache that was defined as a) a reduction in headache by 3 or more in the pain rating scale measured at 1 hour from receiving the initial medication, or b) a major reduction in the severity of headache, defined as a numeric pain rating scale that reached 2/10 or lower. Secondary outcomes were improvement of headache also by a decrease by 3 or more in pain scale measured at 30 minutes and 2 hours. Other details of the study like the choice of initial pain medications by ER physicians, choice of music genre by patients, and need for additional pain medications were also noted.
Statistical methods
Data analysis was performed in Stata SE version 13. Improvement versus non-improvement of pain severity were categorical variables for which fisher exact test was utilized. However, the pain scale was treated as a continuous variable for which t-test was applied. Qualitative variables were tabulated as frequency and percent. The level of significance was set at 0.05, with a power of 80%.
Results
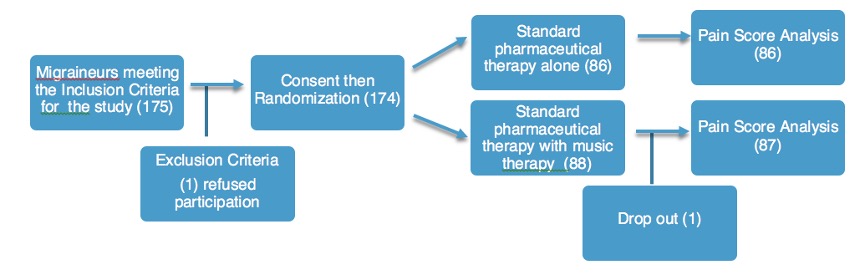
From the period of July 2017 to June 2018, one hundred and seventy-five (175) patients were invited to participate in the study and one patient refused participation. The rest of the 174 participants were randomized to their treatment group. A total of 86 participants received standard medical therapy alone, while 87 participants received medical with MuMed. One participant in the MuMed arm noted irritation to the music 30 minutes into the intervention and noted a progression in the severity of the current headache. The participant then dropped-out of the study. Pain score from both groups were then analyzed. Figure 1 shows a representation of the participant flow.
Figure 1. Participant flow chart
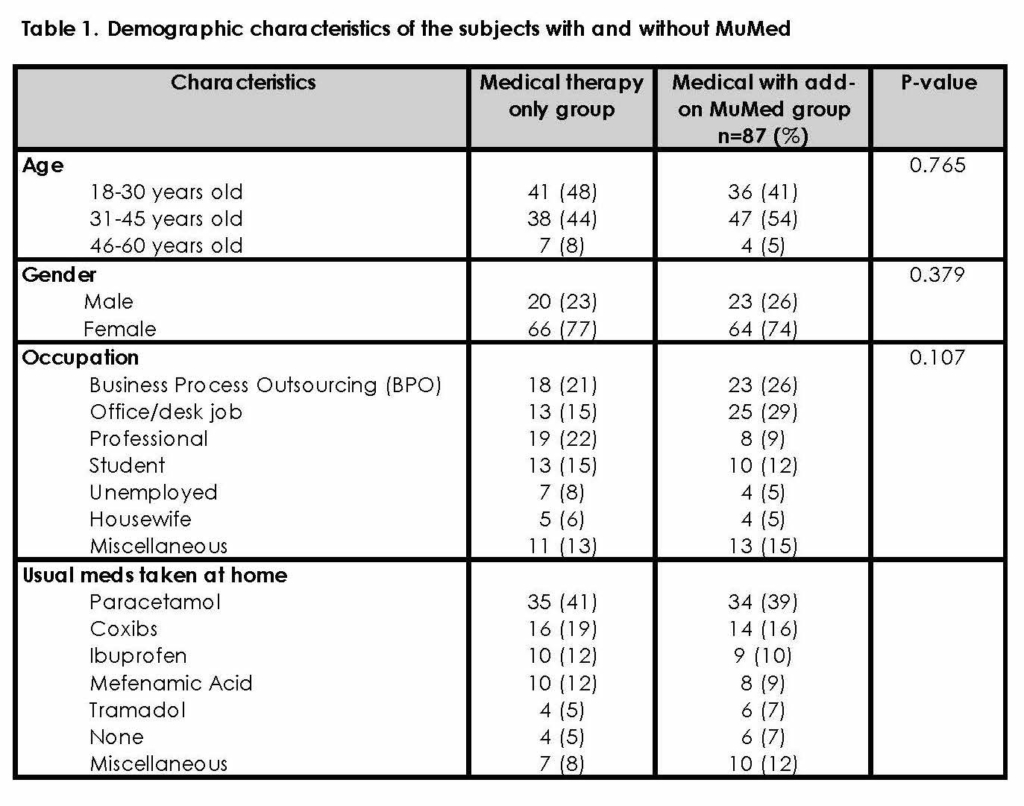
Most of the subjects were between the ages of 18-45 years and three-fourths of the subjects were females. They had varied jobs, but most of them were from the business process outsourcing (BPO) sector followed by office or desk jobs. There were no noted significant differences between the two groups with regard to age (p=0.765), gender (p=0.379), and occupation (p=0.107). As to their usual pain medications taken at home during an attack, most patients took Paracetamol and Coxibs such as Celecoxib and Etoricoxib. Table 1 shows the demographic characteristics of the patients enrolled in the study.
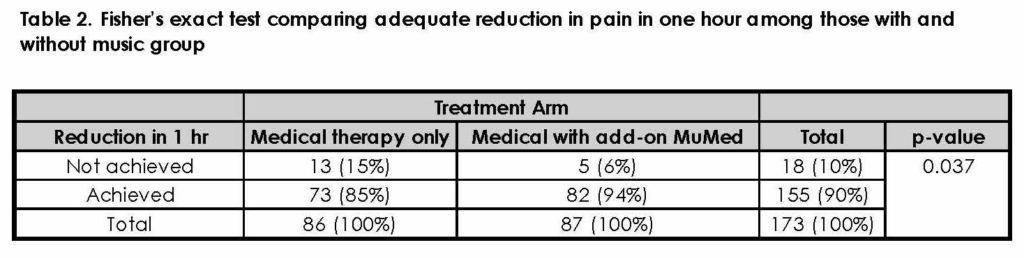
A Fisher’s exact test was performed to determine if there were differences in decreasing the severity of an acute migraine attack based on the treatment arm. The results showed that there was an adequate reduction in the severity of pain after one hour from administration of medicine in 82 out of 87 in the medical with MuMed (94%) as compared to 73 out of 86 in the medical therapy alone (85%), a difference that was statistically significant (P=0.037). Table 2 shows the 2×2 table of the study.
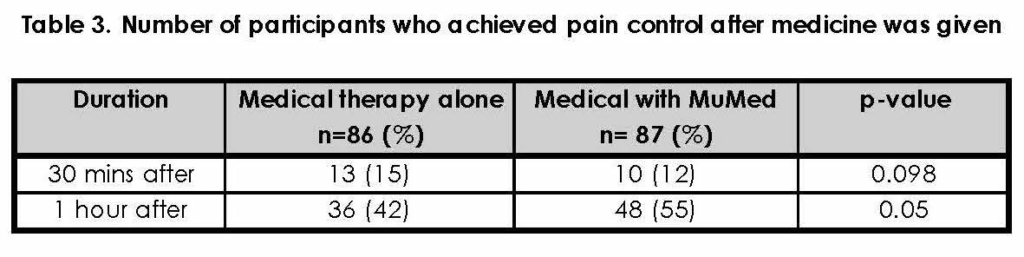
With regards to the duration of headache, 36 of 86 (42%) of those who received medical therapy alone compared to 48 of 87 (55%) of those who received medical with music therapy, had a pain rating of 0-2, an hour after the medicine was given. Table 3 summarizes the data on participants who achieved adequate pain relief.
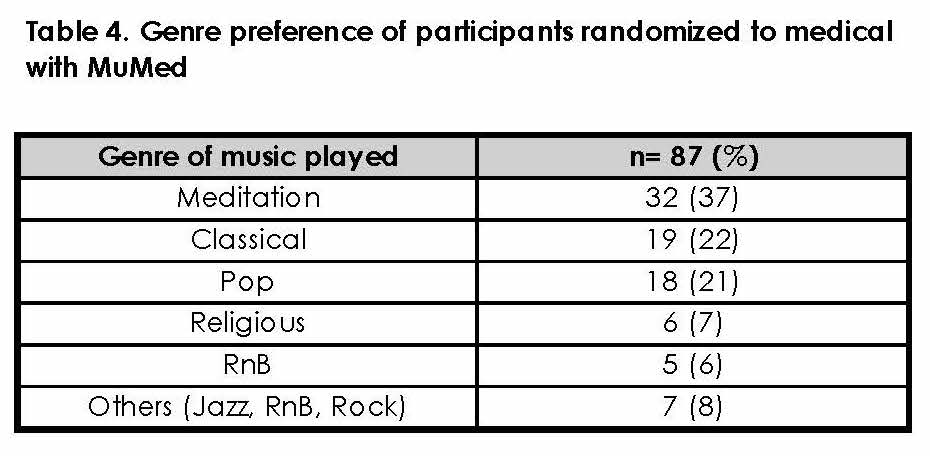
Participants who were randomized to the medical with MuMed were given the option to choose the genre of music they prefer. Based on the selection of participants in this study, one-third chose meditational music (32 of 87, 37%), followed by classical (19 of 87, 22%), and pop music (18 of 87, 21%). Table 4 lists down the participant’s genre choice.
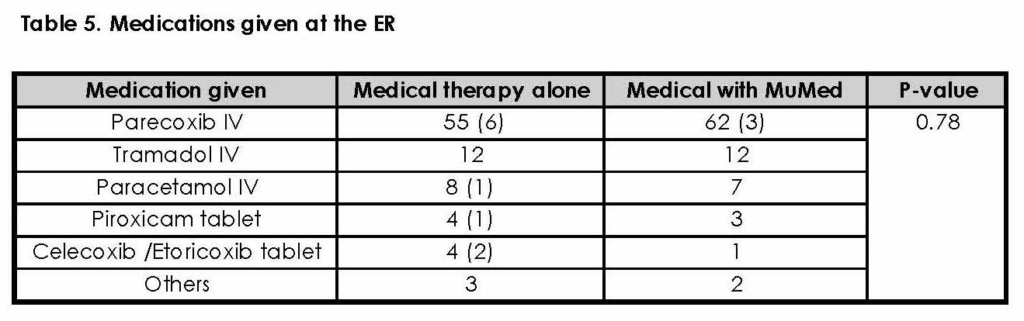
Table 5 shows that at the ER, the most commonly prescribed initial medications for a migraine attack was Parecoxib for both treatment groups, followed by Tramadol and Paracetamol. Fischer’s exact test was performed to determine if there was a difference in decreasing headache severity based on medication used. The results showed there was no significant difference between the two groups, with p=0.780. Only 10 of the participants were given oral pain medications, while the rest were given intravenous pain medications. Enclosed in parenthesis in the table below were those who needed additional pain medications. A total of 13 participants needed additional pain medications after reporting a pain score of 7 or more one hour after medication was given. Of the 13 participants, 10 of those came from the medical therapy alone arm and 3 came from the medical with MuMed treatment arm including the patient who dropped out of the study. Antiemetics were also provided as symptomatic treatment to the participants who presented at the ER with a history of vomiting (62 of 173). Upon enrollment in the study, there was no complaint of vomiting, hence no further antiemetic medications were provided.
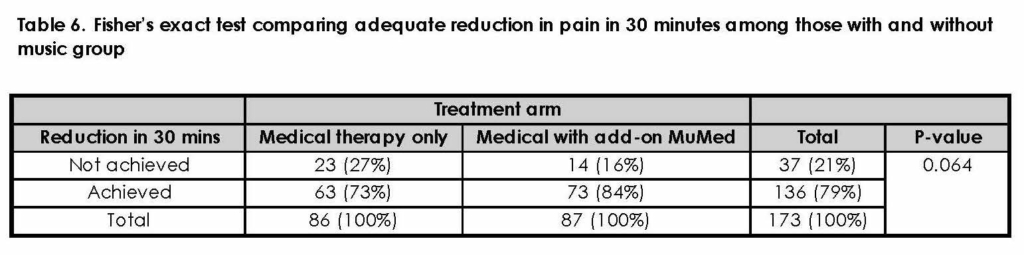
Pain rating after 30 minutes from the administration of medicine was obtained and analyzed. The results showed reduction in the severity of pain 30 minutes after administration of medicine in 73 out of 87 in the medical with MuMed (84%) compared to 63 out of 86 in the medical therapy alone (73%). The difference however was not statistically significant (P=0.064, Fisher’s exact test). Table 6 shows the 2×2 table of the study.
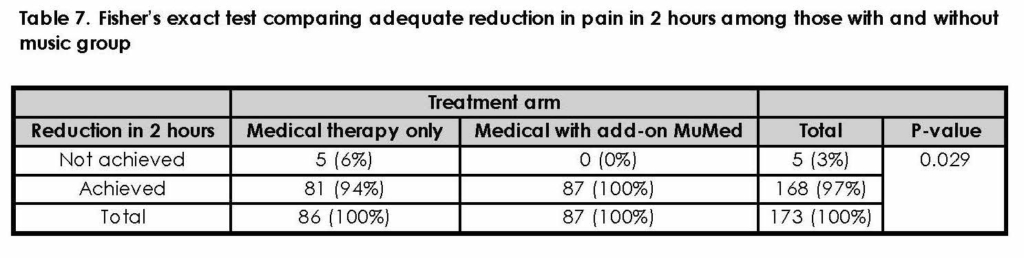
Pain rating after 2 hours was also analyzed and results showed reduction in the severity of pain after 2 hours from administration of medicine on all of the 87 participants in the medical with MuMed (100%) as compared to 81 out of 86 in the medical therapy alone (94%), a difference that was statistically significant (P=0.029, Fisher’s exact test). Table 7 shows the 2×2 table of the study.
By the 2nd hour of the study, 13 participants were already discharged, 11 of which came from the medical with music therapy group.
An independent t-test was done on the particular pain scores (0-10/10) provided by the participants to compare the reduction of pain in one hour among those in medical group vs medical with music group. This was done to identify if a decrease of less than 3 in the numeric pain rating scale will also be significant one-hour post medication. The results showed that participants under the medical with MuMed had statistically significant lower mean pain score (2.63 + 0.19) compared to those under medical therapy alone (3.4 + 0.26), t(171) = 2.40, p = 0.0173.
Discussion
Utilization of music in the management of pain has been reported in various clinical settings like pre-operative surgery, labor pain and as palliative treatment for cancer patients 2, 3, 4, 5. In this paper, the investigators tried to relate MuMed to a common neurologic condition that causes disability in the everyday lives of those affected. They focused on MuMed’s effect in reducing the severity and duration of an acute migraine attack as compared to giving traditional pain medication alone. Since its effect in acute migraine attack has not been established, this prompted a thorough search of MuMed in relation to migraine 4. The investigators searched studies published in PubMed, Cochrane, Medline, Herdin, and Google Scholar. The keywords and strategy used for the search were “migraine OR headache OR distress OR analgesia OR primary headache OR tension type headache OR pain relief OR status migrainosus” AND “music OR music therapy (MT) OR listening” AND “randomized clinical trial (RCT) OR clinical trials OR randomized trials”. After a thorough search, only four studies reported the effectiveness of MuMed in migraine; all of which were done on chronic migraine where one study was done in the adult population, the other in pediatric population, and the other two were on adolescents. The results were varied but most did not show a significant benefit of MuMed on chronic migraine 6. In the meta-analysis by Lee on the effects of music on pain where more than 70 RCTs published from 1995 to 2014 were comprehensively reviewed, there was no report on the effect of MT on acute migraine attacks 9. Up to present, there is still no available reports on the effect of MuMed in the management of pain in an acute migraine attack. This may be partly due to the fact that music therapists do not have access to ER facilities compared to physicians.
Music interventions were categorized as either MT or MuMed. According to Dileo & Bradt, MuMed is defined as “pre-recorded music listening experiences administered by medical personnel” while MT is “a therapeutic process that involves a relationship between a client and therapist” 10. In this study, MT and MuMed were used interchangeably.
Obtaining a consent from a patient in severe pain could possibly raise an ethical issue as it can be presumed that the participant would be unable to give an informed decision in that condition. To remedy this the investigators opted to wait for 15 minutes after the pain medication was given before getting the participant’s consent. This allowed the pain medication to start acting and the patient to be able to settle down.
Another issue that was brought up was the possibility that the presence of noise in any kind, not necessarily music, was enough to have a positive effect on headache reduction. Other RCTs on MuMed employed the use of white noise as a treatment arm to address this problem. However, it was not offered in this study because the investigators found it unfair and unethical to provide a patient with earphones that played white noise only. It was also deemed impractical to play white noise if there was a choice to play music instead.
The demographic characteristics of patients involved in the study were mostly young to mid-adults, with a predominance of females than males, as also noted in the study done by Roxas et al 11. Regarding occupation, BPO centers are currently a common job in the young-mid adult population. It is not surprising that individuals from this line of work are prone to migraine attacks, especially because they work in front of a computer throughout their shift. This is also true for those working in an office or desk job. As for their as-needed pain medications, most of them took paracetamol and coxibs to relieve their headache. These widely available over-the-counter drugs are popular options in any kind of pain, not needing any consult with a physician.
There were also other nonpharmacological therapies studied in relation to acute migraine attack such as psychophysiologic management (biofeedback), self-relaxation, trigger point massage, acupuncture, visual imagery, and transcranial magnetic stimulation 12, 13. These were not studied in this paper.
Adding MuMed to the usual medications given at the E.R. hastened the decreased pain severity. This may be secondary to the inhibition of pain signal transmission through the gate control theory of pain that brings about relaxation and relief of pain provided by Music Therapy. This theory states that pain impulses travel from the site of injury to the brain via the spinal cord where neural gates may be opened or closed, which indicates the level of pain that passes through. Listening to relaxing music causes the gates to close thereby decreasing the pain impulses that reach the brain. Also, the brain releases neurotransmitters in response to musical impulses which in turn stimulates the endocrine glands to release endorphins. These endorphins modulate pain and produces a feeling of euphoria. By inhibiting pain response and stimulating release of endorphins, music makes the patient’s headache better 14.
Participants were given the liberty to choose a genre that they deemed to have a calming effect on them. A controlled randomization of music genre was not performed in this study because the investigators believe that genre or music preference varies from person to person. Therefore, correlation between specific music genre and its effect on pain relief could not be concluded in this study. Self-liberty in selection of music would however eliminate the possibility that an absence of pain relief is secondary to listening to music that they do not like to begin with. Music acted as a distraction for the subjects allowing them to relax, think clearer, and reduce tension. MuMed also reduced anxiety, which was difficult to separate from pain as pain is defined as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage” 15. Achieving a decrease in the severity of pain therefore also shortens the duration of an attack, as seen in Table 3. It can be noted that in an hour from receiving medical therapy, there was a big gap already leaning towards a better, positive outcome in resolving a migraine attack on those who received MuMed as compared to those who did not. There were even 11 patients in the intervention group who were sent home in less than 2 hours because of faster resolution of headache as compared to only 2 patients in the control group. This finding will improve the turnover time of patients seen at the ER and could decrease the admission rate due to acute migraine attacks. The investigators would therefore recommend using MuMed in addressing migraineurs in the ER. Patients can be made aware of the potential benefits of MuMed in achieving faster relief from their headache when they are on their own.
Limitations and Recommendations
This study only measured the pain rating until the second hour of post medication, it would be helpful to know what other interventions were offered to the participants and how long it took them to achieve relief.
Moreover, this is an open label study, participants were aware of their intervention arm, which may contribute to the extent of decrease in pain rating expected from them versus in reality. This study did not include physiologic parameters such as blood pressure, heart rate and respiratory rate as variables that can be indicators of pain.
Songs included in the playlists may not be representative of their genre. They may not be the best options in trying to reduce headache severity. Additionally, this research did not study whether a specific genre is beneficial as an add-on in treating an acute migraine attack. This can be a focus in future trials.
Additional information on the demographics of the patient like identifying those with and without aura, may contribute to the effect of MuMed on the headache severity.
This paper concentrated on MuMed’s effect in acute migraine attack treatment. Future studies can investigate its effect as a migraine prophylaxis.
Conclusion
Filipinos spend a substantial amount of time listening to music. In this study, MuMed showed a positive effect as an add-on to current medical therapy in reducing the severity and duration of an acute migraine attack, both 1- and 2-hours post medication. It is a practical, inexpensive, and readily available add-on component of acute migraine attack management.
References
- Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007 Jan 30;68(5):343-349. PubMed CrossRef
- Gallagher LM, Lagman R, Rybicki L. Outcomes of Music Therapy Interventions on Symptom Management in Palliative Medicine Patients. Am J Hosp Palliat Care. 2018 Feb;35(2):250-257. PubMed CrossRef
- Krishnaswamy P and Nair S. Effect of Music Therapy on Pain and Anxiety Levels of Cancer Patients: A Pilot Study. Indian J Palliat Care. Jul-Sep 2016;22(3):307-11. PubMed CrossRef
- Chuan CH, Chen PC, Lee CCS, et al. Music Intervention for pain and anxiety management of the primiparous women during labout: A systematic review and meta-analysis. J Adv Nurs. 2019 Apr; 75(4):723-733. PubMed CrossRef
- Graff V, Cai L, Badiola I, Elkassabany N. Music Versus midazolam during preoperative nerve block placements: a prospective randomized controlled study. Reg Anesth Pain Med. 2019 Jul 18;rapm-2018-100251. PubMed CrossRef
- Koenig J. Music therapy in the treatment of primary headache disorders. OA Alternative Medicine. 2014 Jan:18;2(1):1. Date accessed: October 23, 2020. URL
- Desiderio L. Spotify changes way Pinoys listen to Music. The Philippine Star. December 9, 2019. Date accessed: October 23, 2020. URL
- Kudrow D, Thomas M, Ruoff G, et al. Valdecoxib for treatment of a single, acute, moderate to severe migraine headache. Headache. 2005 Oct;45(9):1151-1162. PubMed CrossRef
- Lee JH. The effects of music on pain: A meta-analysis. J Music Ther. Winter 2016;53(4):430-477. PubMed CrossRef
- Dileo C, Bradt J. Medical Music Therapy: A Meta-analysis & Agenda for Future Research. Chery Hill, NJ: Jeffrey Books; 2005.
- Roxas A, Gose M, et al. The prevalence of stroke, parkinsonism, dementia, migraine and epilepsy in the Philippine part II: Application of the PNA questionnaire in the 2003 National Nutrition Health Survey. The Philippine Journal of Neurology. June 2007: 11(1): 5-11. Date accessed: October 23, 2020. URL
- Kalra AA, Elliot D. Acute Migraine: Current treatment and emerging therapies. Ther Clin Risk Manag. 2007 Jun; 3(3):449-459. PubMed
- Sarchielli P, Granella F, Prudenzano MP, et al. Italian Guidelines for Primary Headaches: 2012 revised version. J Headache Pain. 2012 May;13(Suppl 2):31-70. PubMed CrossRef
- Krout RE. Music listening to facilitate relaxation and promote wellness: Integrated aspects of our neurophysiological responses to music. Arts Psychother. 2007 Dec;34(2): 134-141. CrossRef
- Task Force on Taxonomy of the International Association for the Study of Pain. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. Merskey H, Bogduk N, editors. 2nd Ed. IASP Press; c1994. 210 p. Date accessed: October 23, 2020. URL
Declarations
Ethics Approval and Consent to Participate
The study was approved by the International Review Board (IRB) of the hospital. The hospital has an IRB with Accreditation Level 3. All subjects were given informed consent forms and were assured of their privacy. Only the principal investigators and statistician had access to the results.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
This research was supported by a research grant provided by The Brain Foundation of the Philippines (BRAIN), Inc.
Prior presentation: Parts of this manuscript were presented as an abstract at the Asian Oceanian Congress of Neurology 2018.
Author’ Contributions
Both authors helped in the conceptualization of the paper. PD wrote the manuscript under the guidance of AR. Both authors read and approved the final manuscript.
Acknowledgement
We would like to thank the Neurology consultants and residents, especially Dr. Liz Edenberg Quiles, who helped in the execution of the protocol and fine-tuning of the research paper. We would also like to acknowledge the E.R. staff, from the E.R. nurses, medical clerks, interns, residents, and the ER consultants who took extra effort in referring to us potential subjects. Thank you to our in-house statistician who helped in the generation of results for this study. This would also not be possible without the financial assistance by The Brain Foundation of the Philippines (BRAIN), Inc.
Disclosures
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
