Author: Aleksandr Isakov MD 2,4, Naum Shaparin MD 1,2,3,4, Jacob Hascalovici MD, PhD *1,2,3,4
Author Affiliation:
1 Multidisciplinary Pain Center, Montefiore Medical Center, Bronx, NY
2 The Saul R. Korey Department of Neurology, Montefiore Medical Center, Bronx, NY
3 The Arthur S. Abramson Department of Physical Medicine and Rehabilitation, Department of Anesthesiology, Montefiore Medical Center, Bronx, NY
4 Albert Einstein College of Medicine, Montefiore Medical Center, Bronx, NY
Research Support: Support was provided solely from institutional and/or departmental sources.
Competing Interests: The author/s declare no competing interests.
Issue: 02.04
DOI: doi.org/10.30756/ahmj.2020.02.04
Received: March 26, 2020
Revised: April 1, 2020
Accepted: April 11, 2020
Published: April 20, 2020
Recommended Citation: Isakov A, Shaparin N, Hascalovicil J. Suspected Status Migrainosus During Flu Season. Ann Head Med. 2020;02:04. DOI: 10.30756/ahmj.2020.02.04
Objective: The following case report is presented to highlight the importance of maintaining a high index of suspicion for secondary causes of headache, especially during influenza season.
Case Report: A 61-year-old woman with a history of infrequent episodic migraine without aura presented to our multidisciplinary pain management center during the flu season with a 1-month history of persistent and continuous headache, suspicious for status migrainosus. Imaging of the brain was obtained to rule out secondary causes of headache and was notable for findings consistent with acute rhinosinusitis.
Conclusion: We discuss a case of headache secondary to acute rhinosinusitis during the flu season presenting as suspected status migrainosus. Herein, we discuss the differential diagnosis of secondary headache of 1-month duration and present the treatment options for headache secondary to acute rhinosinusitis.
Case Report
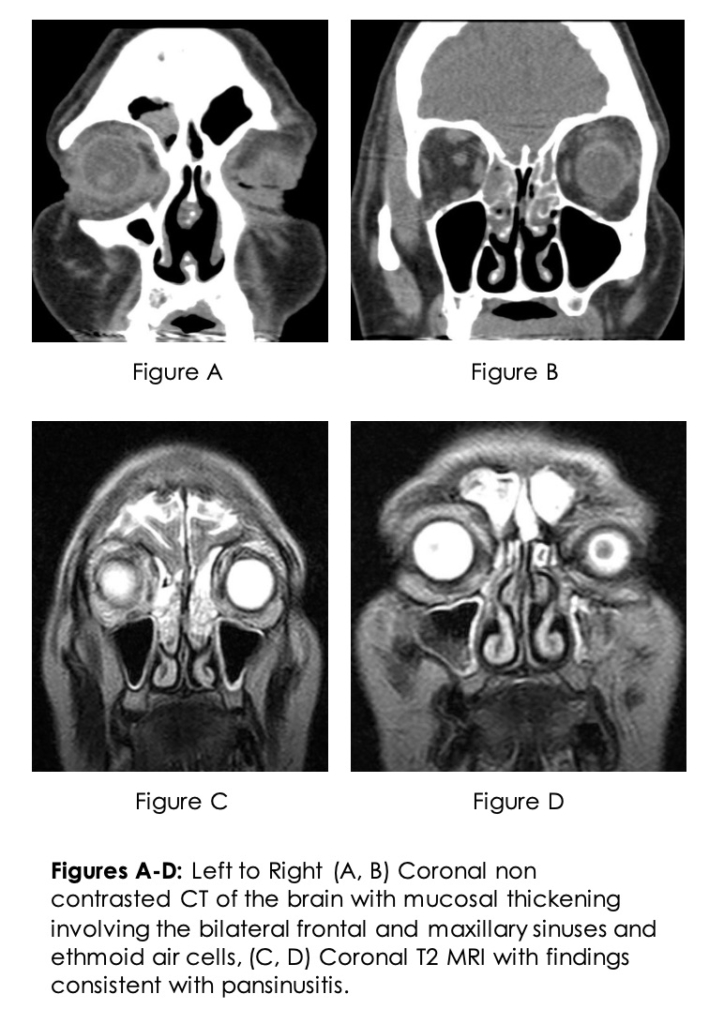
A 61-year-old woman with a history of infrequent episodic migraine without aura presented to our multidisciplinary pain management center during flu season with a 1-month history of persistent and continuous headache, suspicious for status migrainosus. The patient had previously described her migraines as being unilateral occipital and temporal throbbing pain occurring on 2-3 days per month with associated photophobia and phonophobia. Previously, non-steroidal anti-inflammatories (NSAIDs) and acetaminophen were sufficient for acute migraine therapy and the patient was never placed on migraine prevention therapies. The current headache was unlike her prior migraines in that the pain was constant, bifrontal, without photophobia and phonophobia and not responding to oral pharmacotherapy for pain. She reported flu-like symptoms one week prior to the headache onset but otherwise the review of systems was negative. She was treated with intravenous NSAIDs, antiemetic and antihistamine combinations in the emergency department on several occasions with only temporary symptomatic relief. The neurological exam was normal. A non-contrast head and paranasal sinuses computed tomography scan followed by magnetic resonance imaging of the brain was obtained to rule out secondary causes of headache. The results notable for mucosal thickening involving bilateral frontal and maxillary sinuses and ethmoid air cells, consistent with pansinusitis (Figures A-D). The headache resolved with a course of antibiotics.
Discussion
The International Headache Society defines headache caused by acute rhinosinusitis as any headache associated with clinical and or radiological evidence of sinus disease, which develops in temporal relation to rhinosinusitis, is exacerbated by direct pressure over the paranasal sinuses and improves after treatment of the underlying sinus disease.1 Treatment of headache secondary to acute rhinosinusitis may include NSAIDs, anti-congestants and antibiotics in refractory cases.2, 3
Pain with palpation of the paranasal sinuses can be a clinical feature present in both migraine and headache secondary to rhinosinusitis, therefore the latter is often misdiagnosed as migraine.4 Sinusitis is an uncommon complication of all upper respiratory infection (~0.5%) and, influenza being one of the most common causes of sinusitis.5 The differential diagnosis includes primary headache disorders such as new daily persistent headache, tension-type headache and status migrainosus as well as secondary etiologies such as cerebral venous sinus thrombosis, idiopathic intracranial hypertension and intracranial space occupying lesion.6 Interestingly, many patients without any history of migraine who are diagnosed with sinus headache are ultimately diagnosed with migraine.7 We observed the opposite phenomenon wherein a patient with episodic migraine developed rhinosinusitis during influenza season and was initially misdiagnosed as having status migrainosus.
Conclusion
This case illustrates the importance of maintaining a high index of suspicion for secondary causes of headache, especially during influenza season.
References
- Olesen J, et al. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition – Preface. 2018;38(1):5. PubMed CrossRef
- Chiarugi A, Camaioni A. Update on the pathophysiology and treatment of rhinogenic headache: Focus on the ibuprofen/pseudoephedrine combination. Acta Otorhinolaryngol Ital. 2019 Feb;39(1):22-27. PubMed CrossRef
- Eross E, Dodick D, Eross M. The Sinus, Allergy and Migraine Study (SAMS): CME. Headache. 2007 Feb;47(2):213-224. PubMed CrossRef
- Levine H, Setzen M, Holy C. Why the confusion about sinus headache? Otolaryngol Clin North Am. 2014 Apr;47(2):169-174. PubMed CrossRef
- Worrall G. Acute sinusitis. Can Fam Physician. 2011 May;57(5):565-567. PubMed
- Tyagi A. New daily persistent headache. Ann Indian Acad Neurol. 2012 Aug;15(Suppl 1):S62-S65. PubMed CrossRef
- Schreiber CP, Hutchinson S, Webster CJ, et al. Prevalence of migraine in patients with a history of self-reported or physician-diagnosed “sinus” headache. Arch Intern Med. 2004 Sep;164(16):1769-1772. PubMed CrossRef
Disclosures
Consent/Permissions: Patient consent was received to report the case.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
