Author: David A Provenzano MD *1, Samer Narouze MD PhD 2
Author Affiliation:
1 President Pain Diagnostics and Interventional Care, Sewickley, PA
2 Professor and chairman, Center for Pain Medicine, Western Reserve Hospital, Cuyahoga Falls, OH
Research Support: Support was provided solely from institutional and/or departmental sources.
Competing Interests: The author/s declare no competing interests.
Issue: 02.03
DOI: doi.org/10.30756/ahmj.2020.02.03
Received: April 12, 2020
Revised: April 14, 2020
Accepted: April 15, 2020
Published: April 17, 2020
Recommended Citation: Provenzano DA, Narouze S. Telemedicine Healthcare for Headache Medicine During COVID-19 and Beyond. Ann Head Med. 2020;02:03. DOI: 10.30756/ahmj.2020.02.03
The current COVID-19 pandemic sheds light on the importance of telemedicine in the care of patients experiencing headaches. Generally, headache patients suffer from lack of access to healthcare and physicians specializing in headache medicine. Now more than ever, telemedicine is needed during the COVID-19 pandemic to limit unnecessary virus exposure while still providing high-level quality care.
Currently there is no published research regarding the risk of COVID-19 infections in headache patients. Nevertheless, headache patients must follow best practices like the rest of the population to limit their personal risk of infection and to mitigate virus community spread.
During this unprecedented public health crisis, our priority as headache specialists and health care professionals is to support social distancing while ensuring proper access to healthcare. Telemedicine will play a key role in expanding such access to physicians specializing in headache medicine. Furthermore, the expansion of telemedicine initiated during the COVID-19 pandemic will most likely continue once the pandemic ends secondary to documented high levels of acceptability, patient satisfaction, improvements in patient access, and cost of care reductions. The purpose of this manuscript is to define the current utilization of telemedicine for headache patients and to provide strategies for incorporation into headache care plans during the COVID-19 pandemic.
Introduction
Headache care management in the United States and globally has always been challenged by the low number of headache specialists compared to the number of headaches suffers seeking care. Recently, this care gap has been further worsened and highlighted by the restrictions in care during the COVID-19 pandemic. On March 11, 2020, the WHO declared Novel Coronavirus-2019 (COVID-19) as a pandemic.1 Currently as of April 14, 2020 there were 1,970,879 confirmed cases and total of 125,678 deaths.2 Specifically, in United States there were 611,156 confirmed cases with 25,942 deaths. Globally, healthcare systems across the world have been faced with unique challenges for controlling the spread of infection while still maintaining care for non-acute or -emergent patients. Consequently, in-person headache care including procedures and office visits have often been suspended which has impacted the care of patients frequently having complex medical needs. Although telemedicine has been studied in headache patients, widespread adoption has not occurred. Telemedicine will play a vital role in caring for headache patients during the COVID-19 pandemic to limit unnecessary virus exposure and to protect the health of patients, healthcare workers, and the community. The purpose of this manuscript is to define the current utilization of telemedicine for headache patients and to provide strategies for incorporation into headache care plans during the COVID-19 pandemic.
The Burden of Headaches
Often physicians encounter daily patients suffering from headaches in their offices. For example, migraine or severe headaches affect nearly 15% of the United States population which equates to approximately 45 million individuals.3, 4 Migraines affect roughly 1 out of every six to seven Americans annually and this number has remained stable over the last decade. 3, 4 Migraine and severe headaches are costly and associated with high levels of disability. Over 50% of all migraine patients report significant or severe impairment and disability.5 Specifically, migraine is the leading cause of years lived with disability among patients between ages 15 and 49 years old.6 Migraines are a major cause of work-related absenteeism. It is estimated that 8% of patients with episodic migraines and 11% of patients with chronic migraines missed at least 1 day of work per week over the previous 2 weeks.7 Migraines also affect quality of life. Approximately 65-75% of patients with migraine have missed family events and activities including household chores in the past month due to migraine-related impairment.7
Telemedicine Improves Headache Patients’ Access to Healthcare
Currently, it is estimated that there are only approximately 650 certified headache specialists in USA.8, 9 This number of headache specialists is challenged to meet the needs of millions of headache patients seeking medical care. Expectedly, it is not uncommon for headache patients to have long wait times for appointments and to travel long distances to see a specialist. Telemedicine can assist in meeting the clinical care needs of individuals with headaches by improving access and removing barriers that exist in current care models.
Prior to the COVID-19 pandemic significant interest existed in telemedicine as demonstrated by the global telemedicine market being valued at $18.2 billion in 2016 and the estimation that this value would double by 2022.10 Although interest existed and research demonstrated its value, telehealth’s utilization was limited by reimbursement challenges, coverage limitations and technology restrictions. Many of the telehealth benefits demonstrated in general care models, including reducing transfer rates, improving convenience, increasing efficiency, decreasing visit travel and wait times, and reducing costs would also be of benefit to patients suffering from headaches.11, 12, 13
The use of telemedicine for nonacute headache care has been examined. Research to date from randomized and prospective trials demonstrated that telemedicine is not inferior to traditional consultations with regards to clinical outcomes (e.g. Headache Impact Test-6 and pain intensity) compliance levels, and patient satisfaction.14, 15 Specifically for migraines, a one-year randomized controlled trial of a cohort of patients with severe migraine-related disability, showed that telemedicine was a feasible mode of treatment and an effective alternative to in-office visits for follow-up migraine care.16 Clinical outcomes, namely improvement in MIDAS scores, number of headache days, and average headache severity at 12 months for participants in the telemedicine group were not different from those in the in-office group. Convenience was rated higher in the telemedicine group secondary to reduced travel times and decreased absenteeism from work.
One of the inherent limitations of telehealth is the inability to perform an in-person exam. Fortunately, for diagnosis and treatment of headaches, history plays a significant role. In addition, when comparing neurological examinations performed by telemedicine to face-to-face encounters, the telemedicine examination compared favorably in most components of the exam.17 The American Academy of Neurology recently offered a webinar on remote physical examination to provide further education during the COVID-19 pandemic.18 The webinar suggested that a majority of the relevant physical exam could be conducted remotely. The portions of the exam that could not be conducted remotely included funduscopic examination and deep tendon reflexes. Furthermore, vital signs could only be assessed if the patient had the appropriate tools at their home location.
When performing telehealth visits, it is also important to screen for headache red flags indicating a concern for a secondary headache. Concerning systemic and neurologic signs and symptoms that require further evaluation include but are not limited to alterations or loss of consciousness, confusion, fever or weight loss, progressive vision changes, seizure, pulsatile tinnitus, and aphasia.19 If any of these signs or symptoms are present during the telehealth visit, then appropriate in-person care needs to be initiated including possible evaluation in the emergency room.
Telemedicine Implementation During the COVID-19 Pandemic
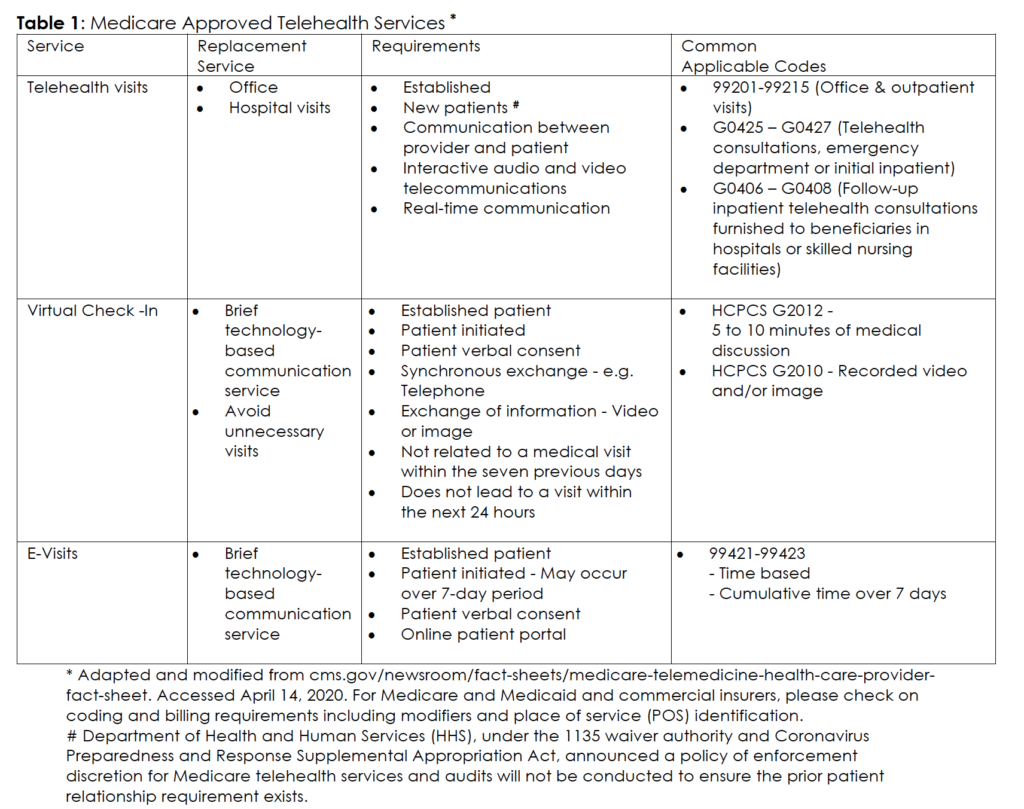
Numerous telehealth pre-existing barriers, such as reimbursement and coverage limitations, have been reduced or eliminated during the COVID-19 pandemic to make this a viable offering to patients suffering from headaches. Under the 1135 Waiver Authority and Coronavirus Preparedness and Response Supplemental Appropriation Act signed into law March 6, 2020, multiple restrictions to telehealth were temporarily removed including: established patient requirement, rural area designation, and place of service requirement. Based on reducing the place of service requirement, now Medicare beneficiaries may receive these services in their homes (Table 1). In addition, the Centers for Medicare and Medicaid Services (CMS) stated that these services would be paid at the same rate as the corresponding level for a regular in-person visit. The Officer of the Inspector General (OIG) on March 17, 2020 notified physicians and practitioners that they will not be subject to administrative sanctions for reducing or waiving any cost-sharing obligations (coinsurance and deductibles) that Medicare beneficiaries may owe for telehealth services provided during the COVID-19 declaration.20
Another challenge that existed with the use of telehealth was the requirement to use a HIPAA compliant communication platform, the US Department of Health and Human Services (HHS) will waive potential penalties for healthcare providers’ HIPPA violations that involve providing telehealth medical services to patients through everyday communication technologies during the COVID-19 nationwide public health emergency.21, 22 Specific communication applications listed in the notification included FaceTime, Skype, Facebook Messenger video chat, Google Hangouts video, and Zoom. Communication strategies that should still be avoided include the public facing platforms: Facebook live, Twitch, and TikTok.
It is also important to recognize the licensure requirements for providing telemedicine in a specific state. Most of state boards require that the physician engaging in telemedicine is licensed in the state in which the patient is located.23 However, many states have temporarily waived in-state licensure requirements during the pandemic. Healthcare providers should continue to check state licensure requirements as they continuously evolve during this time period. Furthermore, a healthcare provider should confirm with their malpractice provider that telehealth is covered service.
Although opioids are generally not a preferred medication for most headache patients, a subset of patients suffering from intractable headaches may occasionally require controlled substances. Since the Secretary of the U.S. Department of HHS has declared a Public Health Emergency, DEA registered practitioners in all areas of the United States may issue Schedule 2 through 5 controlled substances to patients for whom they have not conducted an in-person medical evaluation if specific criteria are met. The specific criteria that need to be met include: the prescription is issued for a legitimate medical purpose by the practitioner in the usual course of treatment, the telemedicine/telehealth communication is conducted using audiovisual, real-time two-way interactive communication system, and the practitioner is acting in the accordance with the applicable federal and state laws and regulations, including opioid prescribing guidelines.24 Although, controlled substances may be provided without a direct in-person medical evaluation, it is still recommended that opioid safe prescribing procedures be performed including assessing for adequate pain control, adverse events, aberrant behavior, and activities improvement.25 Pill counts can still be performed via video communication. Patients should continue to be educated on the risks and benefits of opioids, naloxone should be prescribed when appropriate, and the review of medical history and medications that impact opioid prescribing should be continued.
Another challenge that may be encountered specifically for headache patients suffering from migraines undergoing telehealth appointments is the decision regarding the continuation of OnabotulinumtoxinA injections. When making the decision whether to discontinue these injections, the risks of exacerbation of migraine headaches and possible emergency room/hospital admissions should be carefully weighed. An informed discussion with the patient discussing other preventative therapies including calcitonin gene-related peptide (CGRP) modulating drugs should occur.
Conclusion
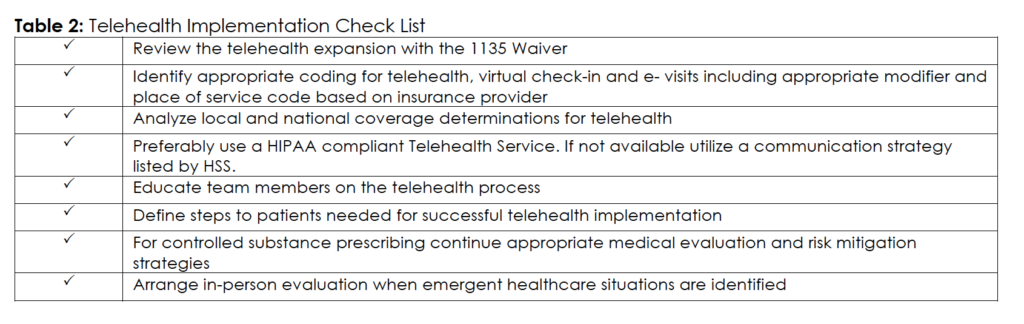
During the COVID-19 pandemic, it is important that physicians continue to provide medical services in a safe and effective way to patients suffering from headaches. Telehealth can help meet the needs of physicians managing and patients receiving care for headaches. In order to increase patient acceptance of these technologies it’s important to explain their benefits and increase their ability and confidence to effectively use these platforms. One of the most important constructs with patients with chronic disease states that positively influence the use of the telehealth technology were their confidence levels.26 Table 2 provides a checklist for the implementation of telehealth. In addition, it is important to remember that many of the waivers and alteration in regulations that have occurred during the COVID-19 pandemic will be reversed once the pandemic resolves. Practitioners must continuously monitor these changes in order to remain in compliance. Although, we suspect that increased integration of telemedicine that occurs during the COVID-19 will further advance and encourage the use of telemedicine in the treatment of patients suffering from headaches.
References
- Shanthanna H, Strand NH, Provenzano DA, et al. Caring for patients with pain during the COVID-19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia. 2020 Apr 7. Pubmed CrossRef
- COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Accessed 4/12/2020. URL
- Burch R, Rizzoli P, Loder E. The Prevalence and Impact of Migraine and Severe Headache in the United States: Figures and Trends From Government Health Studies. Headache. 2018 Apr;58(4):496-505. Pubmed CrossRef
- Burch RC, Loder S, Loder E, Smitherman TA. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. Headache. 2015 Jan;55(1):21-34. Pubmed CrossRef
- Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007 Jan 30;68(5):343-349. Pubmed CrossRef
- Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017 Sep 16;390(10100):1211-1259. Pubmed CrossRef
- Stewart WF, Wood GC, Manack A, et al. Employment and work impact of chronic migraine and episodic migraine. J Occup Environ Med. 2010 Jan;52(1):8-14. Pubmed CrossRef
- Headache Medicine Certification Through United Council for Neurologic Subspecialties. Accessed April 14, 2020. URL
- Headache Medicine Certification Through American Board of Headache Medicine. Accessed 4/12/2020. URL
- Lurie N, Carr BG. The Role of Telehealth in the Medical Response to Disasters. JAMA Intern Med. 2018 Jun 1;178(6):745-746. Pubmed CrossRef
- Powell RE, Henstenburg JM, Cooper G, et al. Patient Perceptions of Telehealth Primary Care Video Visits. Ann Fam Med. 2017 May;15(3):225-229. Pubmed CrossRef
- du Toit M, Malau-Aduli B, Vangaveti V, et al. Use of telehealth in the management of non-critical emergencies in rural or remote emergency departments: A systematic review. J Teleme Telecare. 2019 Jan;25(1):3-16. Pubmed CrossRef
- Soegaard Ballester JM, Scott MF, Owei L, et al. Patient preference for time-saving telehealth postoperative visits after routine surgery in an urban setting. Surgery. 2018 Apr;163(4):672-679. Pubmed CrossRef
- Müller KI, Alstadhaug KB, Bekkelund SI. A randomized trial of telemedicine efficacy and safety for nonacute headaches. Neurology. 2017 Jul;89(2):153-162. Pubmed CrossRef
- Müller KI, Alstadhaug KB, Bekkelund SI. Telemedicine in the management of non-acute headaches: A prospective, open-labelled non-inferiority, randomised clinical trial. Cephalalgia. 2017 Aug;37(9):855-863. Pubmed CrossRef
- Friedman DI, Rajan B, Seidmann A. A randomized trial of telemedicine for migraine management. Cephalalgia. 2019 Oct;39(12):1577-1585. Pubmed CrossRef
- Craig JJ, McConville JP, Patterson VH, Wootton R. Neurological examination is possible using telemedicine. J Telemed Telecare. 1999;5(3):177-181. Pubmed CrossRef
- Telemedicine and Remote Care. Accessed April 14, 2020. URL
- Robblee J, Grimsrud KW. Emergency Department and Inpatient Management of Headache in Adults. Curr Neurol Neurosci Rep. 2020 Mar 18;20(4):7. Pubmed CrossRef
- OIG Policy Statement Regarding Physicians and Other Practitioners That Reduce or Waive Amounts Owed by Federal Health Care Program Beneficiaries for Telehealth Services During the 2019 Novel Coronavirus (COVID-19) Outbreak. Accessed 4/12/2020. PDF
- OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. Accessed 4/12/2020. URL
- Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. Accessed 4/12/2020. URL
- Telemedicine Policies, Board by Board Overview. Accessed 4/12/2020. PDF
- Diversion Control Division COVID-19 Information Page. Accessed 4/12/2020. URL
- Provenzano DA, Viscusi ER. Rethinking the role of opioids in the outpatient management of chronic nonmalignant pain. Curr Med Res Opin. 2014 Oct;30(10):2051-2062. Pubmed CrossRef
- Edwards L, Thomas C, Gregory A, et al. Are people with chronic diseases interested in using telehealth? A cross-sectional postal survey. J Med Internet Res. 2014 May 8;16(5):e123. Pubmed CrossRef
Disclosures
Dr. Samer Narouze is the current EIC for Annals of Headache Medicine. Dr Dmitri Souza was the acting EIC handling this manuscript.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
