Author: Stephania Paredes MD 1, Roderick J. Finlayson MD 2, Samer Narouze MD PhD 3, Sameh M Hakim MD MSc (Pain) MSc (Anesth) PGDipM DipBiostat,MB, BCh 4, Daniel Adams PA-C MSHS DMA 3, Nimish Mittal MBBS MD MSc 5, Michael Catapano BHSc MD 5, Lynn Kohan MD 6, Patrick Connell BSc 3, Nebojsa Nick Knezevic MD PhD 1, Alex Feoktistov MD PhD 7, Imanuel Lerman MD MSc 8, Antoun Nader MD 9, Dmitri Souza MD PhD * 3
Author Affiliation:
1 Department of Anesthesiology, Advocate Illinois Masonic Medical Center, Chicago, IL, USA
2 McGill Alan Edwards Pain Management Unit, McGill University, Montreal, QC, Canada
3 Center for Pain Medicine, Western Reserve Hospital, Cuyahoga Falls, OH, USA
4 Department of Anesthesiology, Intensive Care and Pain Management, Ain Shams University Faculty of Medicine, Cairo, Egypt
5 Faculty of Medicine, Division of Physical Medicine and Rehabilitation, University of Toronto, Toronto, ON, Canada
6 Department of Anesthesiology and Pain Medicine, University of Virginia, Charlottesville, VA, USA
7 Diamond Headache Clinic, Chicago, IL, USA
8 Center for Pain Medicine, UC San Diego Health University of California, San Diego, CA, USA
9 Department of Anesthesiology, Feinberg School of Medicine, Chicago, IL, USA
Research Support: Support was provided solely from institutional and/or departmental sources.
Competing Interests: The author/s declare no competing interests.
Issue: 03.01
DOI: doi.org/10.30756/ahmj.2020.03.01
Received: May 6, 2020
Revised: Jun 29, 2020
Accepted: Jun 30, 2020
Published: Jul 13, 2020
Recommended Citation: Paredes S, Finlayson R, Narouze S, et al. Ultrasound-Guided Cervical Medial Branch Blocks: A Systematic Review and Meta-Analysis. Ann Head Med. 2020;03:01. DOI: 10.30756/ahmj.2020.03.01
Objective:
Cervical medial branch blocks (CMBBs) are useful in differentiating facetogenic pain from other sources of cervicogenic headaches and neck pain. The purpose of this systematic review and meta-analysis is to determine the efficacy, performance time, pain reduction, and adverse events associated with ultrasound (US) guided CMBB compared with other commonly used guidance methods such as fluoroscopy and computed tomography (CT).
Methods:
Searches of MEDLINE, EMBASE, Cochrane Library, and Ovid were completed to identify studies addressing CMBBs utilizing ultrasound compared to other imaging techniques. Three reviewers independently screened the titles, abstracts, and full texts, extracting data from eligible studies. Outcomes of interest including success rate, efficacy, performance time and complication profile were analyzed in meta-analysis. All other reported measures and complication profiles were analyzed descriptively.
Results:
A total of 9 studies were included. Four randomized controlled trials (RCTs) and 5 cohort studies satisfied inclusion criteria. US-guided CMBBs demonstrated similar success rates (OR = 1.05, 95% CI = 0.15 to 7.52, z = 0.05, P = 0.96) and similar pain efficacy (SMD = -0.54, 95% CI = -1.91 to 0.83, z = – 0.77, P = 0.44) compared to traditional guidance techniques. However, US-guided CMBBs demonstrated reduced performance time (SMD = -1.77, 95% CI = -2.65 to -0.89, z = -3.94, P <0.01) and rate of vascular injury/injection (OR = 0.09, 95% CI = 0.01 to 0.75, z = -2.23, P = 0.03) compared to fluoroscopy guided CMBBs.
Conclusion:
This review and meta-analysis demonstrated that US-guided cervical medial branch blocks are a reliable alternative to fluoroscopy- and CT-guided CMBBs, with similar efficacy but a potentially improved safety and performance time.
Introduction
Chronic neck pain is the fourth most common cause of years lived with disability worldwide 1. Nearly 116 million American adults live with neck pain, a higher number than the total affected by cancer, diabetes and heart disease combined 2, 3, 4. Episodes of neck pain commonly subside with or without treatment, although 50% of people continue to suffer from chronic neck pain 5. Lack of timely anatomical diagnosis leads to poor long-term outcomes with conservative treatment of neck pain. Patients with persistent neck pains frequently progress to a trial of a diagnostic block of nerves that supply cervical zygapophyseal joints owing to a lack of valid clinical or radiologic signs for affected joints.
Cervical medial branch blocks (CMBBs) involve anesthetizing the neural supply to the cervical facet joints, typically at several levels 2, 6, 7. These blocks provide essential diagnostic information regarding the anatomic pain generators and predict the response to subsequent radiofrequency ablation that can result in sustained pain relief for up to 12-18-months 2, 6, 7. As such, these procedures necessitate the need for reliability, safety and time efficiency 8, 9, 10.
Traditionally, CMBBs have been performed utilizing either fluoroscopy or computed tomography (CT) to confirm correct needle placement 11. Real-time fluoroscopy with contrast injection is necessary to confirm needle placement and lack of vascular penetration 12, 13, 14. Limited availability of specialized equipment, qualified personnel and associated cost are barriers to widespread use of CT in cervical facet interventions. Ultrasound (US) guidance is an emerging imaging modality in the field of spine interventions that may offer several advantages 7, 15. For instance US guided CMBB: 1) afford for easily accessible machine and or device use, 2) a potential to decrease block performance time, 3) significant reduction in radiation dose and 3) potential reduction in adverse effects due to unintentional intravascular injections 7, 16, 17, 18, 19, 20.
The objective of this systematic review and meta-analysis is to examine the clinical efficacy, performance time, pain reduction, and complication profile of US-guided CMBBs compared to traditional guidance methods of CT or fluoroscopy. We hypothesize that US-guided CMBBs have similar efficacy with improved performance time and reduced adverse events thus serving as a reasonable and safe alternative for the guidance of CMBBs.
Methods
Protocol and registration
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines 21. The review protocol was registered on PROSPERO via study number CRD42020153433 22.
Eligibility Criteria
Studies were included if they were comparison studies reporting the results of CMBB completed under US-guidance (intervention) versus CMBB completed under fluoroscopy or CT-guidance (controls) in adults, >18 years of age, with chronic neck pain. Included studies consisted of randomized control trials (RCTs) and cohort studies reporting: (1) success rate of the block, (2) measure of pain level change after intervention, (3) performance time of CMBB, or (4) adverse effects such as aberrant spread or vascular puncture. Cohort studies and RCTs were chosen to provide the best clinical evidence. Studies classified as: reviews, editorials or technique papers, case reports, animal models or cadaveric studies, and/or studies published in a language other than English were excluded. In addition, studies examining nerve blocks performed at levels other than the cervical spine, studies involving pediatric populations, or studies employing guidance other than US, CT, or fluoroscopy were excluded.
Information sources and searches
MEDLINE, EMBASE, Cochrane Library and OVID were searched from database inception to September 1st, 2019. Initial search was completed on January 1st, 2017 and repeated on September 1st, 2019. Search terms “cervical medial branch block,” “neck pain,” “ultrasound-guided,” and “nerve block” were used.
Study selection
The titles, abstracts, and full texts were reviewed independently and in duplicate by two investigators to determine the relevance of studies (SP, DA). Any discordant articles were reviewed by a third reviewer (DS) to determine the individual article’s eligibility. In addition, the references of included studies were reviewed to identify any additional articles for inclusion.
Data Abstraction
Data abstraction was performed by two reviewers (SP, DA) and reviewed and verified by a third reviewer (DS). Authors of selected articles were contacted via email to collect additional numerical data not available in published manuscripts. If communication with authors was not successful, data were collected through graphics and converted from the available data through standardized formulas presented in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 23.
Quality Assessment
The quality of the included RCTs was assessed using the updated guidelines by the Cochrane Neck and Back Group 24. No scoring system was adopted. Quality assessments were used for descriptive purposes. The risk of bias assessment was performed in the following domains: selection bias (criteria 1, 2, 9), performance bias (criteria 3, 4, 10, 11), attrition bias (criteria 6, 7), detection/measurement bias (criteria 5, 12), reporting bias (criterion 8) and other bias (criterion 13). These domains include all the criterion reported in Cochrane risk of bias tool with additional clarity.
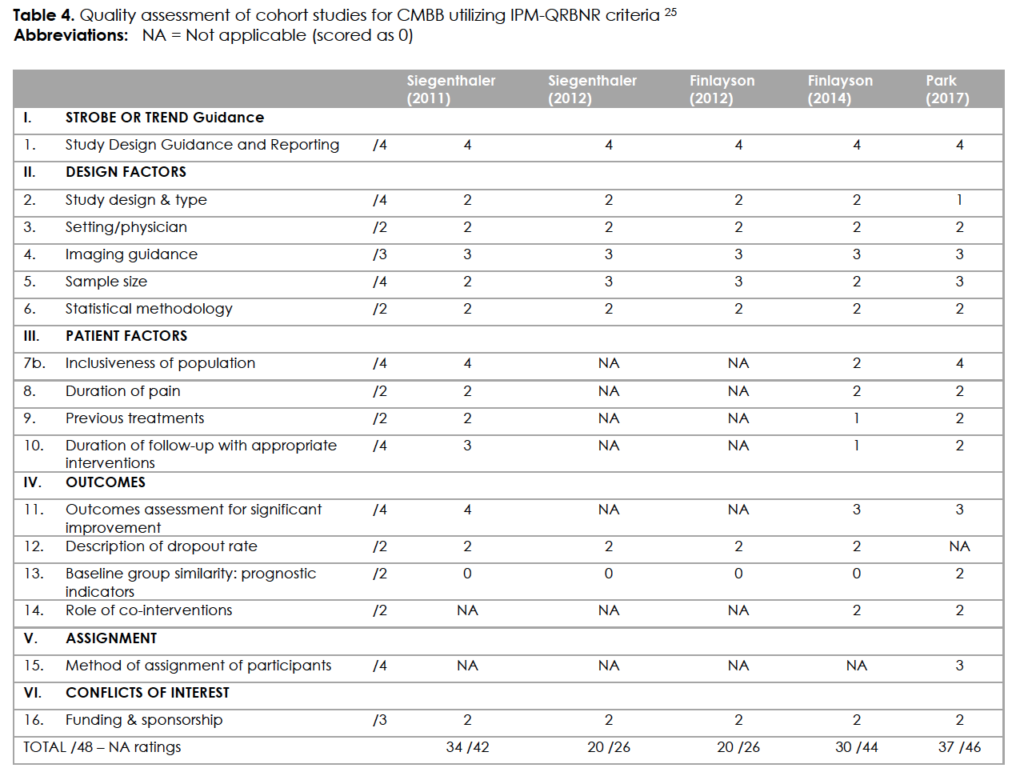
The risk of bias of the individual cohort studies was assessed using the guidelines for methodologic quality assessment of nonrandomized studies of interventional techniques and ROBINS-I 25, 26. This quality assessment was performed by one of the authors (DA) and checked by additional authors (NM and DS). The ROBINS-I assessment tool is designed primarily for cohort studies with interventional and control groups that investigate clinical outcomes. It utilizes the technique of imagining a “target study” to help conceptualize a study’s possible deficiencies compared to an ideal RCT of the same topic. Bias is assessed in seven domains with signaling questions following a standardized format leading to a “triangulation” between similar studies to refine the analysis 26. This is a thorough method which ensures full consideration of the domains in question, but we found that single arm and/or feasibility studies with more technical outcomes were less valid targets of the ROBIN-I. To address this concern, we supplemented the evaluation with the IPM-QRBNR tool, designed specifically for the assessment of bias of pain medicine interventions 25.
Statistical analysis
Statistical analysis was performed using Comprehensive Meta-Analysis® (CMA®) version 2.2.046 (Biostat®, Englewood, NJ). Binary outcomes were compared via estimation of the odds ratios (OR) with 95% confidence interval (CI). Continuous outcomes were compared by calculation of the standardized mean differences (SMDs) and their 95% CI. Estimates from included studies were pooled using the DerSimonian and Laird Random-Effects Method (REM) or the Mantel-Haenszel Fixed-Effects Method (FEM), depending on the presence or absence of significant heterogeneity, respectively.
Sub-group analysis was performed, whenever applicable, by pooling of studies sub-grouped according to the study design (RCT or retrospective) or according to the comparator modality (fluoroscopy or CT) examined versus the US. Point estimates were calculated by pooling of all included studies. Studies included in the meta-analysis were tested for heterogeneity using the Cochran Q Chi-squared test and by calculation of the I-squared (I2) index.
Publication bias was assessed by examination of funnel plots of the estimated effect size on the horizontal axis versus a measure of study size (standard error for the effect size) on the vertical axis. In addition, the Duval and Tweedie Trim and Fill method was used to impute missing studies, if any, and to re-compute an adjusted combined effect.
Results
Search Results and Study Characteristics
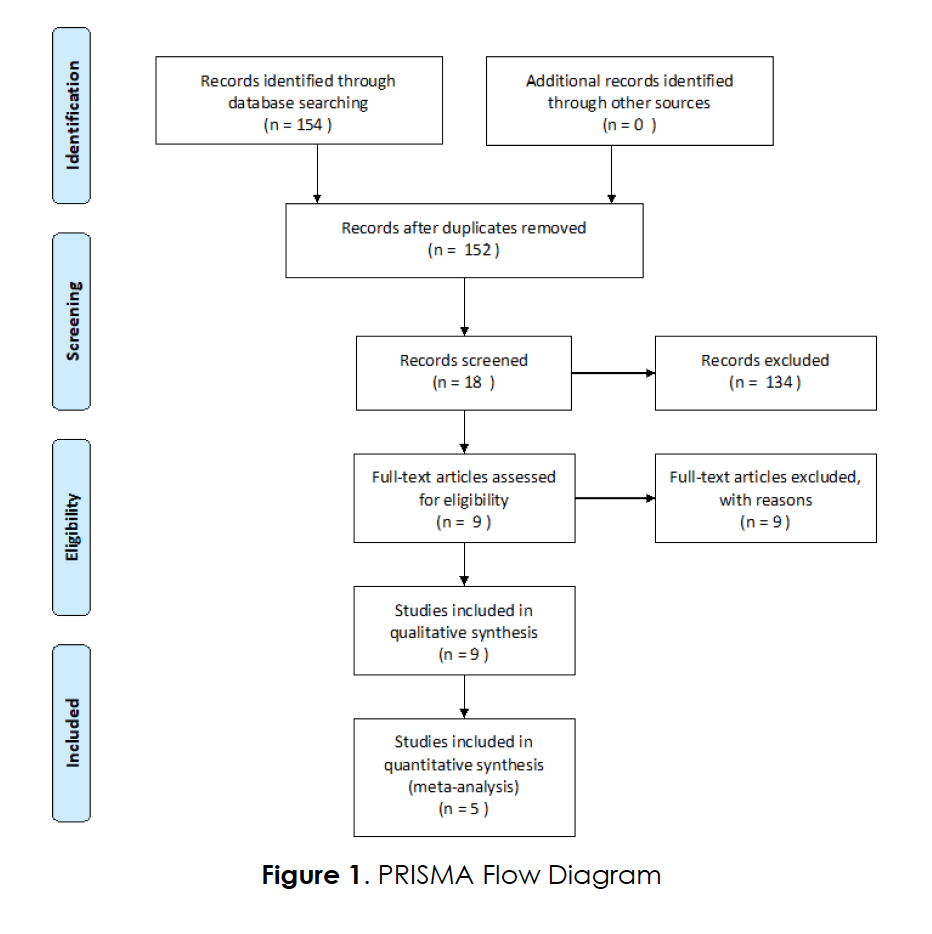
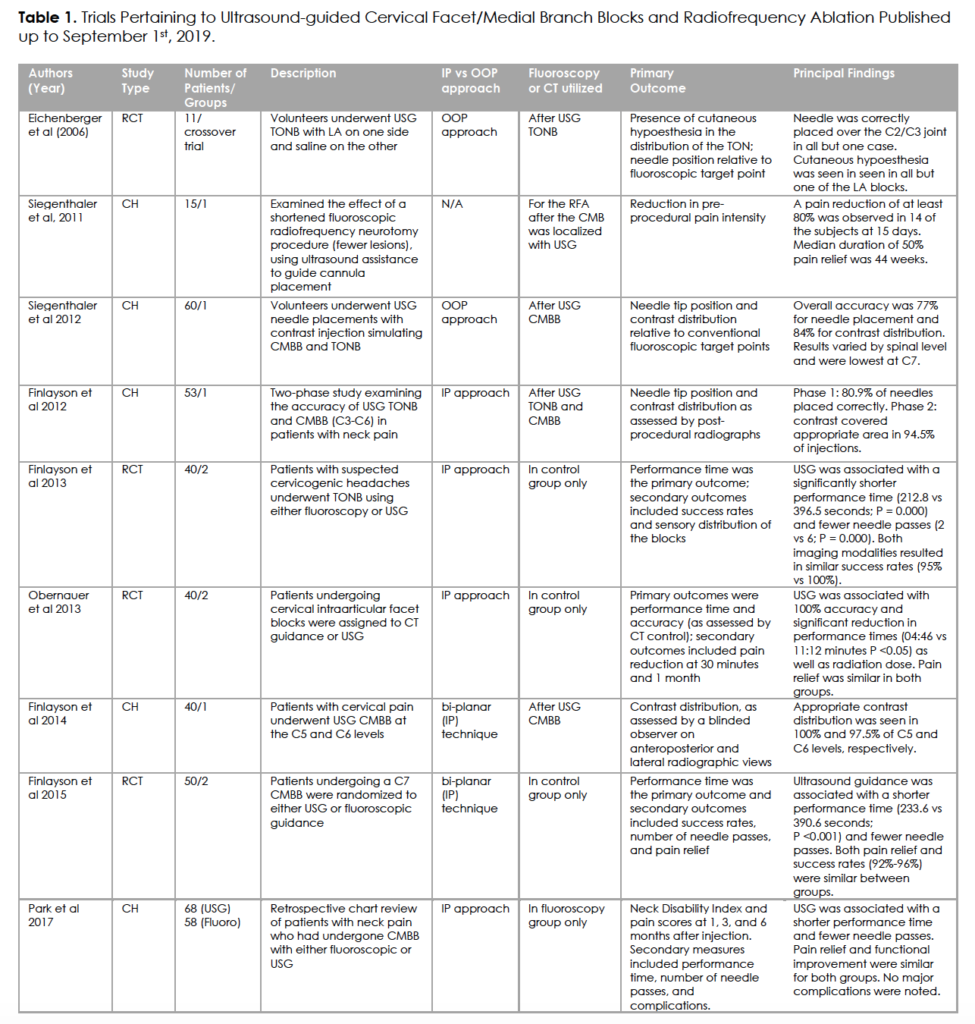
A combined search of MEDLINE, EMBASE, Cochrane Library and OVID yielded 152 results after duplications were removed. Following the title screen, 18 were included in the abstract screening, of which nine progressed to full text review. Nine studies were excluded at the abstract screening stage because they didn’t meet the inclusion criteria, specifically, they did not address cervical medial branch injections. Of the nine studies included, five studies were cohort studies 7, 15, 27, 28, 29 and four studies were RCTs 10, 30, 31, 32 (Figure 1). All studies included in the full text review met eligibility criteria. Five of the 9 studies were included in the meta-analysis. One cohort study 28 was included in the meta-analysis because this study evaluated two comparable groups. Other cohort studies included only one group of patients. No additional articles were retrieved through manual reference search of the included articles. Table 1 summarizes study characteristics, primary outcomes, and principal findings of the studies.
Risk of Bias Assessment
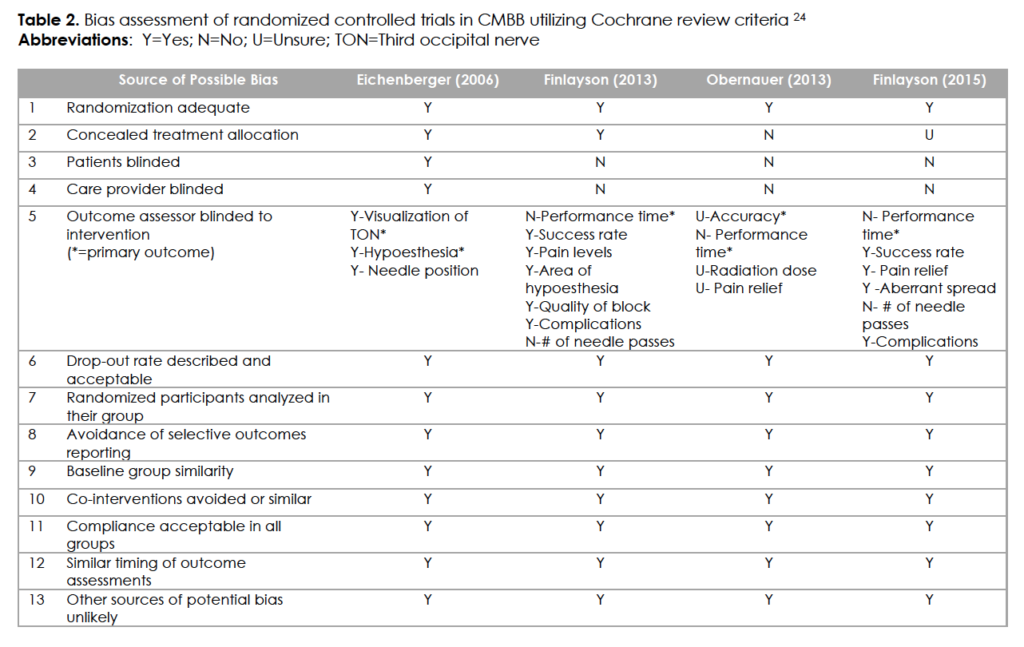
The risk of bias summary for RCTs is presented in Table 2. All RCTs scored a low risk of bias for all the domains except performance bias as three out of four studies did not blind patients or assessors. Data were adequate to examine publication bias for performance time and percentage of pain relief for RCTs. There was no evidence of publication bias regarding either outcome.
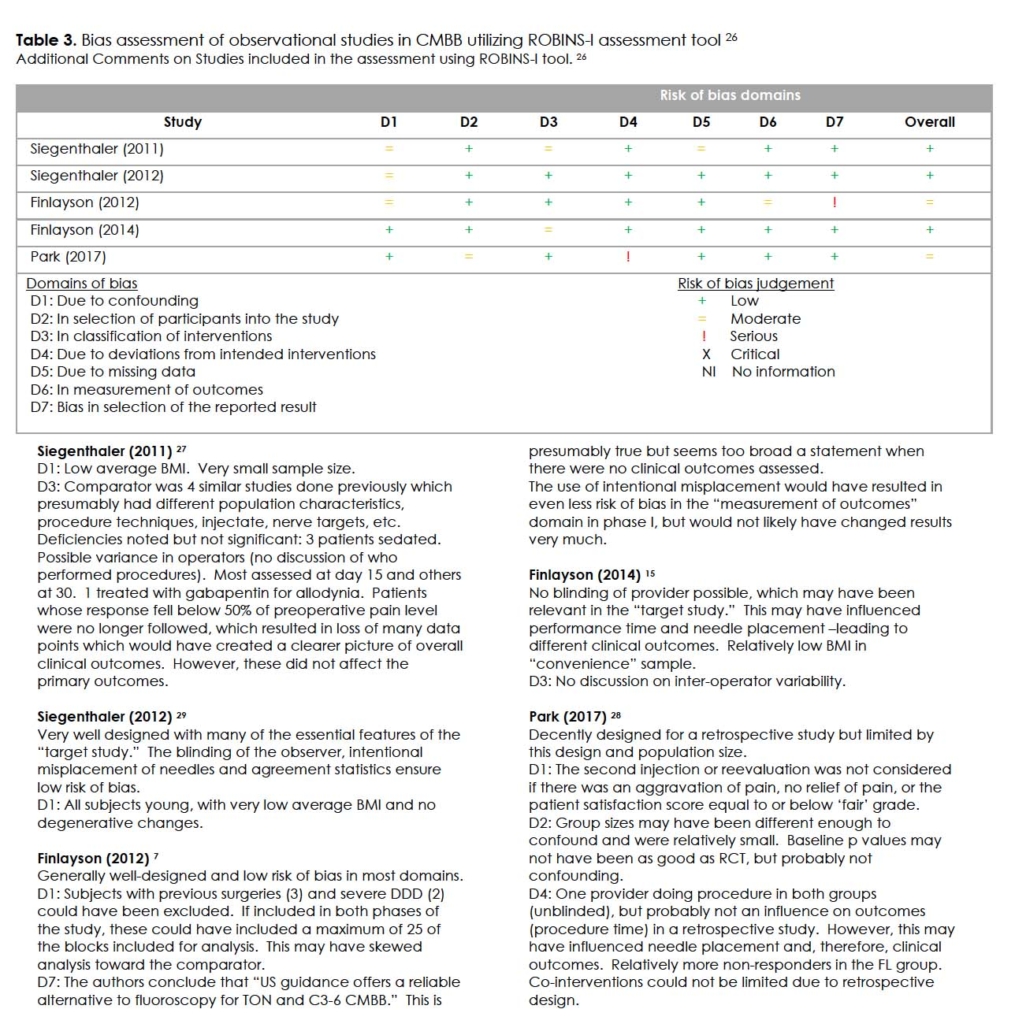
Included cohort studies demonstrated appropriate study design, setting, image guidance, statistical methods, outcome assessment and funding. However, there was generally a privation of cohort studies with regards to assessment and reporting of potential patient factors, including baseline potential prognostic factors or confounders. Two different bias assessment tools for the cohort studies aided to provide a comprehensive view of these studies. The results of cohort studies assessment using ROBINS-I tool 26 presented in Table 3. The results of the assessment with the IPM-QRBNR tool 25 presented in Table 4. The overall risk of bias was found to be low, corresponding to the current trend in pain medicine 33. The specific comments on the individual studies are presented in comments to Table 3.
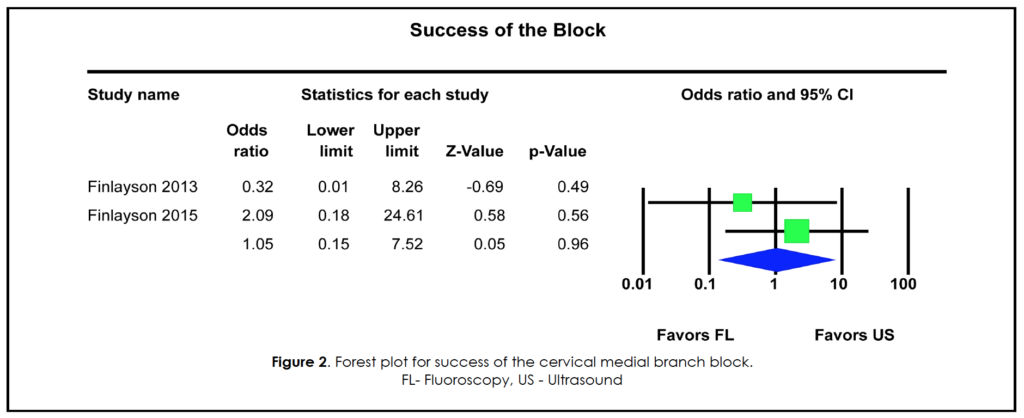
Procedural Success of CMBB under US-guidance
Two RCTs compared CMBB performed with US or fluoroscopy guidance, assessing the correct needle placement for CMBB under each guidance technique 30, 31. A successful block of the third occipital nerve (TONB) was determined as a block that resulted in hypoesthesia of the suboccipital area 30. Alternatively, a successful block of the C7 medial branch, was determined as a block that resulted in the presence of contrast agent continuous with the contour of the C7 superior articular process and covering the entire length and proximal half of the transverse process in an anterior-posterior view 31.
In both studies, the success rates were similar for the standard technique using fluoroscopy guidance and investigative technique utilizing US guidance with no statistically significant difference between groups. Pooling of included studies using FEM demonstrated no statistically significant difference between US- or fluoroscopy-guidance, with an OR for successful block of 1.05, 95% CI = 0.15 to 7.52, z = 0.05, P = 0.96. These results (Figure 2) indicate no difference in success rates comparing the US- and fluoroscopy -guidance.
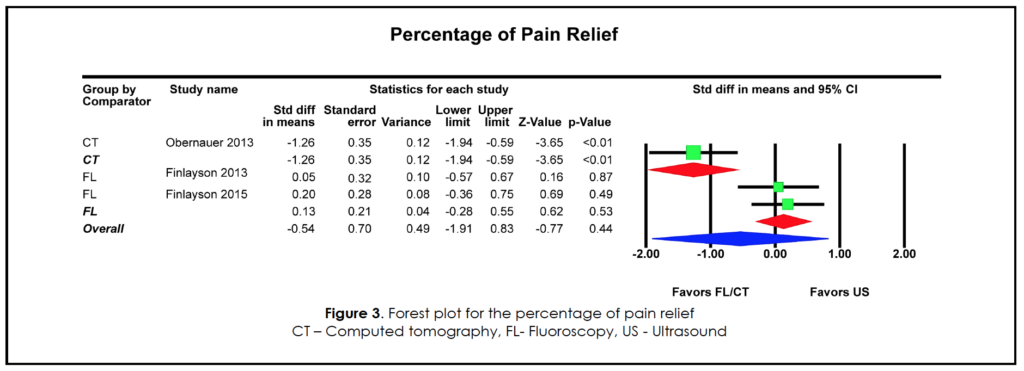
Percentage of pain relief
Three RCT’s reported pain scores before and after CMBB, one utilized a Visual Analogue Scale (VAS) while two others utilized a Numerical Rate Scale (NRS) 30, 31, 32. Individual studies did not demonstrate a statistical difference in pain relief between standard guidance methods and US-guidance. Pooling of included studies using REM demonstrated no statistically significant difference no statistically significant difference between US and all (US vs CT vs Fluoro) standard guidance techniques (SMD = -0.54, 95% CI = -1.91 to 0.83, z = – 0.77, P = 0.44). Sub-group analysis comparing US and fluoroscopy demonstrated no statistically significant difference between the modalities as well (SMD = 0.13, 95% CI = -0.28 to 0.55, z = 0.62, P = 0.53) (Figure 3).
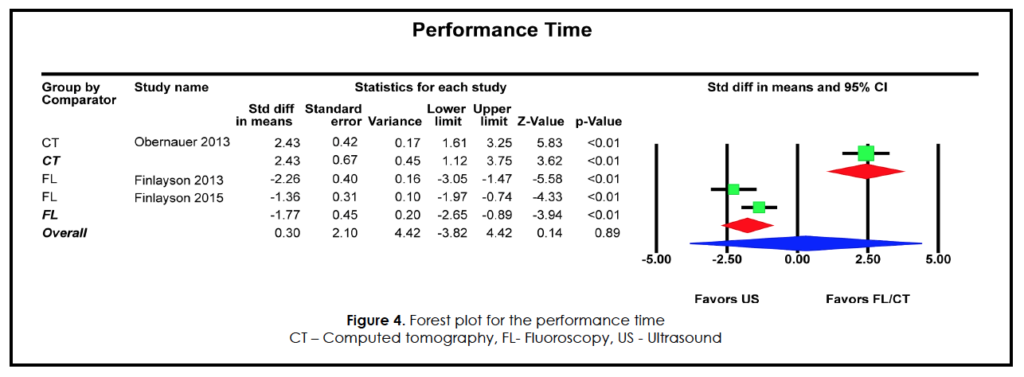
Performance time
Three included studies described procedure performance time utilizing the US versus standard imaging techniques 30, 31, 32. The time was recorded for US from initial skin contact following the application of sterile US gel until the procedure was “successfully complete,” as determined by the sonographer detecting placement of the needle tip directly at the inter-articular space or facet joint and completion of the injection. For CT, the elapsed time was measured from the first CT scan until confirmation of the correct needle position on the final confirmation scan. For fluoroscopy, performance time was measured as the interval between the first radiograph and the end of injection.
Compared to both fluoroscopic imaging and CT, the US-guided procedure was associated with significantly shorter performance times in each individual study. Pooling of all guidance techniques versus US-guidance using REM demonstrated no statistically significant difference in performance time (SMD = 0.30, 95% CI = -3.82 to 4.42, z = -0.14, P = 0.89) (Figure 4). However, sub-group analysis showed shortened CMBB performance time with US-guidance when compared to CMBB with fluoroscopic-guidance (SMD = -1.77, 95% CI = -2.65 to -0.89, z = -3.94, P <0.01).
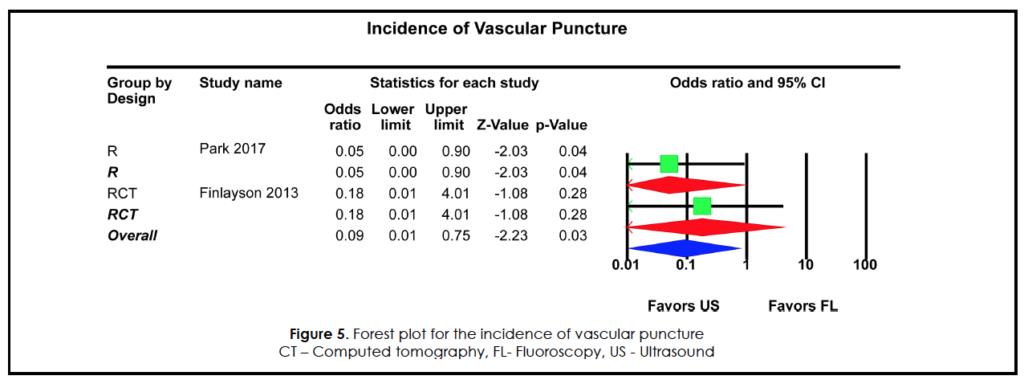
Incidence of vascular puncture
Two included studies reported the incidence of vascular injection 28, 30. The vascular puncture was defined as the aspiration of blood prior to the injection of local anesthetic during either US or standard techniques. Of the two included studies, both reported a benefit with US-guidance, with a fewer cases of vascular puncture due to early identification of vessels under ultrasound guidance and, therefore, prevention of puncture (Figure 5). Meta-analysis of the included studies demonstrated a significantly reduced rate of vascular injections with US-guidance compared to fluoroscopy-guidance (OR = 0.09, 95% CI =0.01 to 0.75, z = -2.23, P = 0.03).
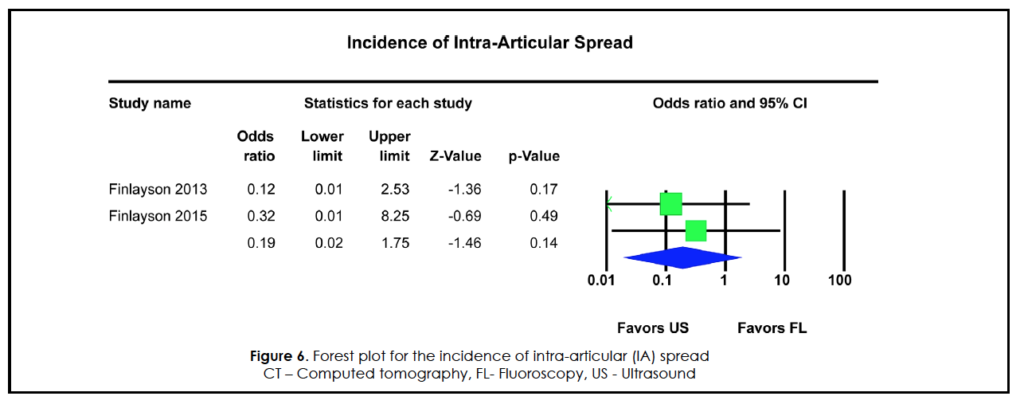
Additional outcomes
Additional outcomes of the incidence of intra-articular injection, intra-foraminal injection, or other aberrant spread were analyzed. Two included studies reported the incidence of unintentional intra-articular injection 30, 31. Meta-analysis of studies reporting TON blocks and CMBBs demonstrated no statistically significant difference between US-guidance and fluoroscopy guidance (OR = 0.19, 95% CI = 0.02 to 1.75, z = -1.46, P = 0.14 (Figure 6) 30, 31. Only one study reported data on intra-foraminal or other aberrant spread. Odds Ratio was completed comparing US-guidance and fluoroscopy guidance, which showed no statistically significant difference between US and fluoroscopy 31.
Discussion
This systematic review and meta-analysis demonstrate that US-guided CMBB is a reliable alternative to fluoroscopy and CT guidance with similar procedure success rates and pain relief level. US-guided CMBB also shown a significant potential to with significant potential to improve performance time and decrease risk of vascular injury. Moreover, there was no increase in aberrant spread of local anesthetic with the use of US-guided CMBB compared to other guidance techniques.
The wide-spread applicability of US including ease of accessibility and convenience as well as increase in the patient safety secondary to a reduction of radiation exposure, and the ability to visualize soft tissues and vascular structures, make US a promising tool for guiding nerve 8, 9, 10, 34, 35. The findings of this systematic review and meta-analysis, are in line with previously published work demonstrating reliability of US-guided CMBB compared with fluoroscopy and CT guidance techniques. Finlayson and colleagues 15 concluded that US-guided CMBB is efficacious, efficient and safe. Ultrasonographic guidance was associated with an effective block at a frequency of 100% and 97.5% for C5 and C6 levels, respectively. Park et al 28 retrospectively compared the outcomes of CMBB performed with either US or fluoroscopy guidance in 126 patients with 6-months follow up. Pain scores and functional status improved similarly in both groups during the study period, and no complications were noted. It was also suggested that US offers dynamic real‐time imaging of the cervical spine facets and surrounding tissue, therefore avoiding the need to continuously adjust the C‐arm to obtain a true lateral view of the cervical spine necessary to correct parallax effects 36.
The ability to identify and avoid vessels in the trajectory of the needle is an important advantage of US-guided cervical spine interventions 30, 36, 37, 38. Cohen et al reported a 7% incidence of unintentional intravascular injections during fluoroscopically guided CMBBs 39. Ultrasonography is a valuable tool for detecting and, hence, preventing vascular injury during CMBBs, whereas contrast fluoroscopy can only demonstrate that the tip of the needle is intravascular, after the penetration of the vessel 37. Cervical vessel penetration and/or injection can cause intravascular thrombosis 40 and other potentially life-threatening complications, including stroke 41, 42, 43. It was hypothesized 37 that fluoroscopy may not detect that the needle has already traversed a vessel on its way to the target, whereas ultrasonography may help avoid this complication. Our systematic review and meta-analysis demonstrated that the rate of accidental puncture of paraspinal vessels was reduced. In addition, 10% of fluoroscopically guided cases were associated with vascular breach compared with no cases in the US-guided group 30.
While the success rate of TON and CMBBs, which were determined by the presence or absence of hypoesthesia in the suboccipital area, were similar between fluoroscopy and US-guidance (95%-100%), the performance times were significantly shorter with US guidance 30.
Another advantage of US-guided cervical facet and medial branch injections, in addition to shorter procedure time compared to fluoroscopy, is an option to insert only one needle 44. Since the cervical medial branches and the TON have variable anatomy, it was suggested to place more than one needle to accommodate the anatomic variability and ensure targeting the selected nerve, when the procedure is performed under fluoroscopic guidance 45. The location of both the TON and the lower cervical medial branches showed significant craniocaudal location variability from their proposed bony landmarks, which are the C2/3 joint cleft for the TON and the deepest point of the articular pillar for the C3–C6 medial branches 44, 46. An upper limit craniocaudal range of 2.2 mm has been documented at the C4 level 46. Real-time ultrasonography allows visualization of the TON and cervical medial branches in most cases and allows for the use of a single needle, which is of benefit to both patient and physician 44. Even if the TON is not well visualized, the C2/3 articulation is typically obvious. Eichenberger et al 10 examined accuracy of needle position over the C2/C3. The investigators performed TON blocks in 10 volunteers using a transverse (short-axis view) and needle out-of-plane approach. They reported accurate needle position over the C2/C3 joint in 82% of blocks (as verified by fluoroscopy) and a success rate of 90%, as determined by the presence of hypoesthesia in the suboccipital area 10.
As in C2/C3 level procedures, our findings were that C7 CMBB completed under fluoroscopic imaging was associated with significantly longer performance times, more needle passes, and a higher incidence of vascular breach compared to US imaging 31, 44. While fluoroscopically guided CMBBs at C7 level pose unique challenges, the ultrasound-guided technique at this particular level is no exception 44. C7 medial branches were visualized on sonography in only one‐third of cases 46. Not surprisingly, a case of iatrogenic spinal cord injury from an US-guided C7 CMBB was reported 47. This was the first, and, to the best of our knowledge, the only serious injury from the US-guided CMBBs. The authors confirmed previous concerns that extreme caution should be emphasized with the performance of certain cervical procedures, including CMBB at the C7 level, independently of the imaging modality used 29, 31, 40, 44, 46. Some experts suggest to use US scanning before the planned procedure 37, 44 to help with the diagnosis of identifying underlying conditions, including facet joint effusions or vascular malformations. The pre-injection scanning can be performed in the short‐axis view to identify blood vessels in the vicinity of the target structure, and then, during the procedure, the needle can be placed in the same view to avoid such blood vessels 44.
Although US-guidance is well established for CMBB, there has been only a single clinical study that has examined the use of US guidance for radiofrequency ablation (RFA) 27. The feasibility of US-guided cervical medical branch RFA was initially proposed by Lee an co-authors 48. Siegenthaler et al examined the effect of US assistance to refine cannula positioning and reduce the number of lesions performed during fluoroscopy-guided RFA. In a cohort of 15 patients, they demonstrated that accurate detection of the nerve under US guidance could decrease the number of lesions and performance time 27. Kim et al reported two successful cases of pulsed RFA performed at C2/3 levels 49.
All studies comparing US-guided cervical interventions with fluoroscopy and CT-guided procedures emphasize the absence of radiation exposure with US guidance 37, 44, 45, 49, 50, 51, 52. Radiation‐free imaging is particularly important with cervical interventions because of increased scattered radiation from the C‐arm 44, 53. Only one group of authors chose to dismiss the risks of radiation exposure during cervical interventional procedures, suggesting that the level of radiation, with appropriate protection, is low 54. It is necessary to emphasize that while the radiation exposure during the cervical interventions is considered to be below the conventional yearly limits, it can lead to appalling sequelae years later, including cell damage and genetic mutations, and, therefore, should be avoided if possible 55, 56.
The similarity in efficacy demonstrated in this review compared to traditional guidance techniques in combination with the intrinsic benefits of US, may increase the availability of CMBB in those with chronic neck pain and decrease the time to intervention that may translate to improved overall quality of life in patients with chronic neck pain 7, 8, 16, 30, 37, 57. Finally, US-guided CMBB reduced risk for vascular injection/injury. US-guided CMBB, therefore, provides a safe option for chronic pain patients and physicians 7, 16, 18, 19, 20, 58. A recent narrative review 54 suggested, without adequate evidence, that ultrasound-guided cervical injections “confers a unique risk profile” including spinal cord injury. In contrast, this rare, but devastating complication is not unique for ultrasound-guided injections 12, 13, 14. Our systematic review and meta-analysis support the efficacy and safety of US-guided CMBBs.
One of the limitations of US-guided CMBB, similarly to any interventions, including fluoroscopy- or CT-guided procedures, is that any of these procedures require proper training. While basic training in US-guided injections may help learn how to visualize the tip of the needle, specialized training is necessary for verifying the levels of the cervical spine. This particular skill is essential for safe and effective US-guided CMBB.
Even though the rigorous methodology of this review (comprehensive literature search, screening process, and thorough assessment of bias) strengthens the conclusions outlined above 21, 23, 24, 26, there are limitations inherent in such an analysis. Limitations are the heterogeneity of the included studies, limited inclusion criteria, and variability of the outcomes reported. In addition, this paper is limited by the small number of studies published and the need for mixed study inclusion, including both RCTs and cohort studies. Despite the high quality of few RCTs included, the addition of cohort studies may introduce additional bias and necessitates the need for further RCTs. Although several RCTs were included, the methodologies, including comparison guidance technique and outcomes reported, were variable and resulted in reduced numbers of papers included in each meta-analysis. This study demonstrates the usefulness and safety of US as a guidance technique for CMBBs. Additional high-quality RCTs are needed to further assess the subgroups of patients, including obese individuals, the elderly, and patients with advanced degenerative changes.
Conclusions
Current evidence suggests that US-guided cervical medial branch blocks may serve as feasible alternative to fluoroscopy-guided and/or CT-guided procedures. US-guided CMBB nerve blocks demonstrated similar efficacy, as well as potentially improved performance time safety compared to fluoroscopy-guided and/or CT-guided procedures. There was no increase in aberrant spread of local anesthetic with the use of US-guided CMBB compared to other guidance techniques. US-guided CMBBs demonstrated significantly decreased the risk of vascular injury. These findings, in addition to the inherent benefits of US compared to traditional imaging guidance techniques, can influence the growth of sonography as a promising imaging guidance modality for nerve blocks and denervation procedures. Additional high-quality clinical trials are needed to further assess the subgroups of patients, including obese individuals, the elderly, and patients with advanced degenerative changes. Although US has the potential to increase the safety of CMBB, specialized training is necessary to obtain expected outcomes, as success, similar to fluoroscopy- and CT-guided interventions, is operator dependent 15, 37, 44.
References
- Hoy D, March L, Woolf A, et al. The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014 Jul;73(7):1309-15. PubMed CrossRef
- Kim PS. Role of injection therapy: review of indications for trigger point injections, regional blocks, facet joint injections, and intra-articular injections. Curr Opin Rheumatol. 2002 Jan;14(1):52-7. PubMed CrossRef
- Boswell MV, Shah RV, Everett CR, et al. Interventional techniques in the management of chronic spinal pain: evidence-based practice guidelines. Pain Physician. 2005 Jan;8(1):1-47. PubMed
- Carrino JA, Morrison WB, Parker L, et al. Spinal injection procedures: volume, provider distribution, and reimbursement in the U.S. medicare population from 1993 to 1999. 2002 Dec;225(3):723-9. PubMed CrossRef
- Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. 2015 Feb;90(2):284-99. PubMed CrossRef
- Galiano K, Obwegeser AA, Bale R, et al. Ultrasound-guided and CT-navigation-assisted periradicular and facet joint injections in the lumbar and cervical spine: a new teaching tool to recognize the sonoanatomic pattern. Reg Anesth Pain Med. May-Jun 2007;32(3):254-7. PubMed CrossRef
- Finlayson RJ, Gupta G, Alhujairi M, et al. Cervical medial branch block: a novel technique using ultrasound guidance. Reg Anesth Pain Med. Mar-Apr 2012;37(2):219-23. PubMed CrossRef
- Galiano K, Obwegeser AA, Bodner G, et al. Ultrasound-guided facet joint injections in the middle to lower cervical spine: a CT-controlled sonoanatomic study. Clin J Pain. Jul-Aug 2006;22(6):538-43. PubMed CrossRef
- Galiano K, Obwegeser AA, Bodner G, et al. Ultrasound-guided periradicular injections in the middle to lower cervical spine: an imaging study of a new approach. Reg Anesth Pain Med. Jul-Aug 2005;30(4):391-6. PubMed CrossRef
- Eichenberger U, Greher M, Kapral S, et al. Sonographic visualization and ultrasound-guided block of the third occipital nerve: prospective for a new method to diagnose C2-C3 zygapophysial joint pain. Anesthesiology. 2006 Feb;104(2):303-8. PubMed CrossRef
- Gangi A, Dietemann JL, Mortazavi R, et al. CT-guided interventional procedures for pain management in the lumbosacral spine. May-Jun 1998;18(3):621-33. PubMed CrossRef
- Verrills P, Nowesenitz G, Barnard A. Penetration of a cervical radicular artery during a transforaminal epidural injection. Pain Med. 2010 Feb;11(2):229-31. PubMed CrossRef
- Heckmann JG, Maihofner C, Lanz S, et al. Transient tetraplegia after cervical facet joint injection for chronic neck pain administered without imaging guidance. Clin Neurol Neurosurg. 2006 Oct;108(7):709-11. PubMed CrossRef
- Edlow BL, Wainger BJ, Frosch MP, et al. Posterior circulation stroke after C1-C2 intraarticular facet steroid injection: evidence for diffuse microvascular injury. 2010 Jun;112(6):1532-5. PubMed CrossRef
- Finlayson RJ, Etheridge JP, Tiyaprasertkul W, et al. A prospective validation of biplanar ultrasound imaging for C5-C6 cervical medial branch blocks. Reg Anesth Pain Med. Mar-Apr 2014;39(2):160-3. PubMed CrossRef
- Obernauer J, Galiano K, Gruber H, et al. Ultrasound-guided versus Computed Tomography-controlled facet joint injections in the middle and lower cervical spine: a prospective randomized clinical trial. Med Ultrason. 2013 Mar;15(1):10-5. PubMed CrossRef
- Greher M, Kirchmair L, Enna B, et al. Ultrasound-guided lumbar facet nerve block: accuracy of a new technique confirmed by computed tomography. Anesthesiology. 2004 Nov ;101(5):1195-200. PubMed CrossRef
- Loizides A, Gruber H, Peer S, et al. A new simplified sonographic approach for pararadicular injections in the lumbar spine: a CT-controlled cadaver study. AJNR Am J Neuroradiol. 2011 May;32(5):828-31. PubMed CrossRef
- Loizides A, Peer S, Plaikner M, et al. Ultrasound-guided injections in the lumbar spine. Med Ultrason. 2011 MAr;13(1):54-8. PubMed
- Loizides A, Obernauer J, Peer S, et al. Ultrasound-guided injections in the middle and lower cervical spine. Med Ultrason. 2012 Sep;14(3):235-8. PubMed
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. PubMed CrossRef
- Souza D, Adams D. Imaging modalities for cervical facet blockade PROPSERO2020. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020153433. Accessed April 2, 2020.
- Li T, Higgins JPT, Deeks JJ (editors). Chapter 5: Collecting data. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. https://training.cochrane.org/handbook. Accessed July 12, 2020.
- Furlan AD, Malmivaara A, Chou R, et al. 2015 Updated Method Guideline for Systematic Reviews in the Cochrane Back and Neck Group. Spine (Phila Pa 1976). 2015 Nov;40(21):1660-73. PubMed CrossRef
- Manchikanti L, Hirsch JA, Heavner JE, et al. Development of an interventional pain management specific instrument for methodologic quality assessment of nonrandomized studies of interventional techniques. Pain Physician. May-Jun 2014;17(3):E291-317. PubMed
- Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. 2016 Oct 12;355:i4919. PubMed CrossRef
- Siegenthaler A, Eichenberger U, Curatolo M. A shortened radiofrequency denervation method for cervical zygapophysial joint pain based on ultrasound localization of the nerves. Pain Med. 2011 Dec;12(12):1703-9. PubMed CrossRef
- Park KD, Lim DJ, Lee WY, et al. Ultrasound versus fluoroscopy-guided cervical medial branch block for the treatment of chronic cervical facet joint pain: a retrospective comparative study. Skeletal Radiol. 2017 Jan;46(1):81-91. PubMed CrossRef
- Siegenthaler A, Mlekusch S, Trelle S, et al. Accuracy of ultrasound-guided nerve blocks of the cervical zygapophysial joints. 2012 Aug;117(2):347-52. PubMed CrossRef
- Finlayson RJ, Etheridge JP, Vieira L, et al. A randomized comparison between ultrasound- and fluoroscopy-guided third occipital nerve block. Reg Anesth Pain Med. May-Jun 2013;38(3):212-7. PubMed CrossRef
- Finlayson RJ, Etheridge JP, Tiyaprasertkul W, et al. A randomized comparison between ultrasound- and fluoroscopy-guided c7 medial branch block. Reg Anesth Pain Med. Jan-Feb 2015;40(1):52-7. PubMed CrossRef
- Obernauer J, Galiano K, Gruber H, et al. Ultrasound-guided versus computed tomography-controlled periradicular injections in the middle and lower cervical spine: a prospective randomized clinical trial. Eur Spine J. 2013 Nov;22(11):2532-7. PubMed CrossRef
- Park J, Mukhdomi T, Kendall M, Oliveira G. Publication Bias in Pain Literature 2019. http://www.asaabstracts.com/strands/asaabstracts/abstract.htm?year=2019&index=3&absnum=1067 Accessed April 2, 2020.
- Pekkafahli MZ, Kiralp MZ, Basekim CC, et al. Sacroiliac joint injections performed with sonographic guidance. J Ultrasound Med. 2003 Jun;22(6):553-9. PubMed CrossRef
- Galiano K, Obwegeser AA, Bodner G, et al. Real-time sonographic imaging for periradicular injections in the lumbar spine: a sonographic anatomic study of a new technique. J Ultrasound Med. 2005 Jan;24(1):33-8. PubMed CrossRef
- Jee H, Lee JH, Kim J, et al. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skeletal Radiol. 2013 Jan;42(1):69-78. PubMed CrossRef
- Narouze SN. Ultrasound-guided cervical spine injections: ultrasound “prevents” whereas contrast fluoroscopy “detects” intravascular injections. Reg Anesth Pain Med. Mar-Apr 2012;37(2):127-30. PubMed CrossRef
- Narouze SN, Vydyanathan A, Kapural L, et al. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. Jul-Aug 2009;34(4):343-8. PubMed CrossRef
- Cohen SP, Strassels SA, Kurihara C, et al. Randomized study assessing the accuracy of cervical facet joint nerve (medial branch) blocks using different injectate volumes. 2010 Jan;112(1):144-52. PubMed CrossRef
- Rathmell JP, Michna E, Fitzgibbon DR, et al. Injury and liability associated with cervical procedures for chronic pain. 2011 Apr;114(4):918-26. PubMed CrossRef
- Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. 2003 May;103(1-2):211-5. PubMed CrossRef
- Benny B, Azari P, Briones D. Complications of cervical transforaminal epidural steroid injections. Am J Phys Med Rehabil. 2010 Jul;89(7):601-7. PubMed CrossRef
- Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. 2001 Apr;91(3):397-9. PubMed CrossRef
- Narouze SN, Provenzano DA. Sonographically guided cervical facet nerve and joint injections: why sonography? J Ultrasound Med. 2013 Nov;32(11):1885-96. PubMed CrossRef
- Govind J, King W, Bailey B, Bogduk N. Radiofrequency neurotomy for the treatment of third occipital headache. J Neurol Neurosurg Psychiatry. 2003 Jan;74(1):88-93. PubMed CrossRef
- Siegenthaler A, Schliessbach J, Curatolo M, Eichenberger U. Ultrasound anatomy of the nerves supplying the cervical zygapophyseal joints: an exploratory study. Reg Anesth Pain Med. Nov-Dec 2011;36(6):606-10. PubMed CrossRef
- Park D, Seong MY, Kim HY, Ryu JS. Spinal Cord Injury During Ultrasound-Guided C7 Cervical Medial Branch Block. Am J Phys Med Rehabil. 2017 Jun;96(6):e111-e4. PubMed CrossRef
- Lee SH, Kang CH, Lee SH, et al. Ultrasound-guided radiofrequency neurotomy in cervical spine: sonoanatomic study of a new technique in cadavers. Clin Radiol. 2008 Nov;63(11):1205-12. PubMed CrossRef
- Kim ED, Kim YH, Park CM, et al. Ultrasound-guided Pulsed Radiofrequency of the Third Occipital Nerve. Korean J Pain. 2013 Apr;26(2):186-90. PubMed CrossRef
- Lord SM, Barnsley L, Wallis BJ, McDonald GJ, Bogduk N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. N Engl J Med. 1996 Dec 5;335(23):1721-6. PubMed CrossRef
- McDonald GJ, Lord SM, Bogduk N. Long-term follow-up of patients treated with cervical radiofrequency neurotomy for chronic neck pain. 1999 Jul;45(1):61-7; discussion 67-8. PubMed CrossRef
- Barnsley L. Percutaneous radiofrequency neurotomy for chronic neck pain: outcomes in a series of consecutive patients. Pain Med. Jul-Aug 2005;6(4):282-6. PubMed CrossRef
- Giordano BD, Baumhauer JF, Morgan TL, Rechtine GR. Cervical spine imaging using standard C-arm fluoroscopy: patient and surgeon exposure to ionizing radiation. Spine (Phila Pa 1976). 2008 Aug 15;33(18):1970-6. PubMed CrossRef
- Schneider B, Popescu A, Smith C. Ultrasound Imaging for Cervical Injections. Pain Med. 2020 Jan 1;21(1):196-197. PubMed CrossRef
- Choi EJ, Go G, Han WK, Lee PB. Radiation exposure to the eyes and thyroid during C-arm fluoroscopy-guided cervical epidural injections is far below the safety limit. Korean J Pain. 2020 Jan 1;33(1):73-80. PubMed CrossRef
- Andreassi MG. The biological effects of diagnostic cardiac imaging on chronically exposed physicians: the importance of being non-ionizing. Cardiovasc Ultrasound. 2004 Nov 22;2:25. PubMed CrossRef
- Fishman SM, Smith H, Meleger A, Seibert JA. Radiation safety in pain medicine. Reg Anesth Pain Med. May-Jun 2002;27(3):296-305. PubMed CrossRef
- Greher M, Scharbert G, Kamolz LP, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. 2004 May;100(5):1242-8. PubMed CrossRef
Acknowledgement
Prior presentation
Parts of the work have been presented at a previous congress or meetings, including International Headache Congress in Dublin, Ireland (2019), American Society of Regional Anesthesia, Pain Medicine Meeting in New Orleans, LA (2019) and American Academy of Pain Medicine Meeting in National Harbor, Washington DC, USA (2020)
Disclosures
Dr. Samer Narouze is the current EIC for Annals of Headache Medicine. Dr Magdalena Anitescu was the acting EIC handling this manuscript.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
